Iowa Cancer Plan
Introduction
Two in five Iowans will be diagnosed with cancer in their lifetime.
Cancer is a complex and costly disease, and addressing it is difficult to do alone. The Iowa Cancer Consortium helps Iowans develop partnerships, find funding, and build skills and knowledge to reduce the burden of cancer. Learn more about becoming a member at canceriowa.org/membership.
To support communities across the state, the Iowa Cancer Plan was created to provide direction and support for those who want to work collectively to reduce the burden of cancer. The plan encompasses the entire cancer control continuum, including actions to reduce the risk of developing cancer or finding cancer early, all the way through treatment and survivorship care.
Goals:
- Health Equity: identify and eliminate cancer health disparities.
- Prevention and Risk Reduction: whenever possible, prevent cancer from occurring.
- Early Detection and Screening: promote the benefits of screening tests to ensure early diagnosis.
- Diagnosis and Cancer-Directed Therapy: reduce barriers to care, promote evidence-based practices and encourage participation in clinical trials and other forms of research.
- Survivorship and End-of-Life Care: ensure resources to optimize quality of life for cancer survivors and their families.
The Impact of COVID-19
There’s no doubt that the 2023-2027 Iowa Cancer Plan was written in a very different social, political, economic, and health care climate than its predecessor. This is due in large part to the COVID-19 pandemic.
At the onset of the pandemic, cancer patients were some of the most vulnerable Iowans. It was crucial then more than ever that health care and public health organizations, along with partners like the Iowa Cancer Consortium, show cancer patients that they would be supported and cared for. Early concerns included vulnerability due to compromised immune systems, further reduced access to transportation and lodging, and deepened financial insecurity.
Now, nearly three years later, we start to see the macro level, systematic impact the pandemic has had on cancer prevention, care, treatment, quality of life, and equity. For example, due to COVID-19:
- Roughly 9.4 million cancer screenings were missed or deferred throughout the U.S.
- Cancer treatments and diagnoses were delayed.
- Cancer clinical trial enrollment decreased by as much as 50%, potentially setting back important scientific finding related to cancer treatment and care.
- Burnout and job loss enlarged already significant workforce issues within health care and public health.
- Existing disparities in health, cancer care, prevention, and social determinants were amplified and deepened.
- At the same time that the criticality of health care and public health was brought newly to the attention of many, distrust deepened for others, strengthening divides.
At the release of the 2023 Iowa Cancer Plan, we are really not yet through the pandemic, and we will not know the extent of effects for some time to come. Though you will see traces of pandemic effects expressly identified throughout this plan, all of the priorities, goals, and actions within should be viewed through the most current lens. Individuals and organizations who implement pieces of this plan should seek the most up-to-date data and be informed by the rapidly shifting social, political, and economic forces that seem to define these “new” times.
And above all, move forward collaboratively, because we are stronger together.
How to use the plan
The Iowa Cancer Plan is intended for use by all cancer control professionals throughout the state, including health care providers and administrators; public health professionals; academics; representatives of community, nonprofit, and advocacy organizations; volunteers; and many others.
Each section includes priorities, strategies, and specific action steps which may be tailored to many settings to guide cancer control activities.
Chapter 1
Health Equity
Chapter 1 Overview
Select a priority to learn more
- Priority 1 Increase the coalition’s capacity to reduce the burden of cancer for all Iowans.
- Priority 2 Increase the number of Iowans with access to quality health care.
- Priority 3 Prioritize health improvement approaches which engage, center, and benefit populations and communities at highest risk of health-related inequities.
- Priority 4 Optimize the cancer care and research workforce to be diverse, reflect the communities served, and meet the needs of all people with cancer and those at risk for cancer, ensuring they live longer and healthier lives.
Identify and eliminate health disparities.
Health equity is when everyone has an equal opportunity to be as healthy as possible.
When applied to cancer, equity means everyone has an equal opportunity to prevent cancer, detect cancers early, and receive treatment and follow-up as soon as possible.
Unfortunately, many Iowans experience challenges to make healthy choices because of other factors — like where they live, their race or ethnicity, gender, sexual orientation, culture, language, education, physical or mental abilities, or income. These differences in health among groups of people that are linked to social, economic, geographic, or environmental disadvantages are known as health disparities.
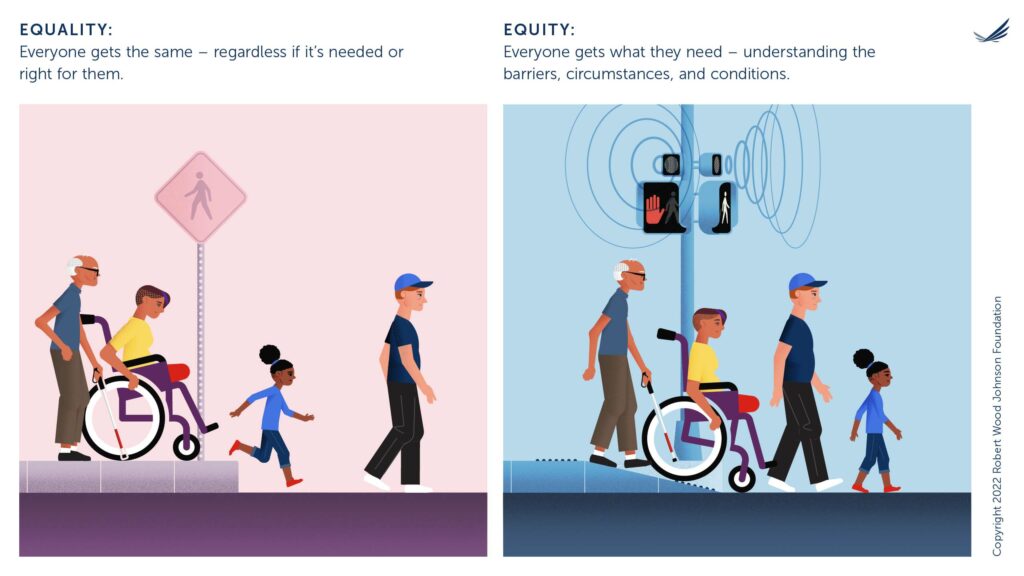
Image: Side-by-side illustrations show four pedestrians of various races, genders, ages, and people with disabilities attempting to cross an intersection. Structural barriers prevent some from crossing on the left entitled “equality”. In the “equity” illustration, a curb cut and accessible pedestrian signals provide safe passage.
A Note about the Social Determinants of Health
The places where people live, learn, work, and play can affect their chances of getting and dying from cancer. These conditions are called social determinants of health. Examples of social determinants of health include a person’s ability to access:
- A good education.
- Healthy food.
- A safe home to live in.
- Reliable transportation.
- Health care.
- Clean water and air.
Stories from the Iowa Cancer Plan
Priority 1: Increase the coalition’s capacity to reduce the burden of cancer for all Iowans.
Strategy A: Increase diversity and engagement of Iowa Cancer Consortium members and partners.
Action Steps:
- Recruit members and partners representing diverse backgrounds and viewpoints including racial and ethnic minorities, tribal nations, the LGBTQ+ community, behavioral health organizations and coalitions or individuals representing Iowans with physical and/or cognitive disabilities.
- Ensure geographic representation across the state, including Iowa’s rural communities.
- Maintain low-cost and scholarship options for Iowa Cancer Consortium membership.
- Engage non-traditional stakeholders in cancer control work including worksites, for-profit organizations, faith-based organizations, and behavioral health agencies.
- Conduct an evaluation of the coalition membership every two years to assure all communities and sectors are represented.
- Build relationships across the state to recognize and include underrepresented individuals and communities in the development and implementation of cancer control activities.
Strategy B: Build upon existing health equity work to deepen existing relationships and extend an organization’s partnerships into communities.
Action Steps:
- Create inclusive virtual and physical spaces.
- Identify and change institutional and structural systems which promote or reinforce activities, behaviors, attitudes, and biases that contribute to inequitable cancer outcomes.
- Increase awareness among the public and health providers about the social determinants of health and their influence on cancer rates.
- Acknowledge the layers of historical trauma which have contributed to a particular community’s mistrust and distrust of the public health and health care systems, and work to heal that trust.
- Engage and center communities at highest risk of health-related inequities when working on health improvement and cancer control activities.
- When possible, use evidence-based strategies and activities to reduce bias, discrimination, and racism within organizations or contribute to the body of knowledge in this space.
- Provide culturally and linguistically appropriate services and education, specifically for populations experiencing health disparities.
- Adopt trauma-informed care policies, practices, and procedures that screen for trauma.
Priority 2: Increase the number of Iowans with access to quality health care.
Strategy A: Promote access to comprehensive health insurance coverage.
Action Steps:
- Ensure Iowans can identify a primary care provider.
- Encourage all Iowans to schedule schedule annual wellness visits with their primary care provider to discuss prevention strategies and deliver recommended clinical preventive services.
- Link Iowans to public and private insurance plans for adults, including Iowa Medicaid.
- Promote and increase awareness of Iowa’s public and private insurance plans for children including the Children’s Health Insurance Program (CHIP) offered through the Healthy and Well Kids in Iowa program (Hawki), which offers health coverage for uninsured children of working families.
- Educate the public about how to access government-sponsored health insurance programs.
Strategy B: Promote access to health and cancer care programs for people who are uninsured or underserved.
Action Steps:
- Promote the Vaccines for Children (VFC) program to provide no-cost vaccinations to Medicaid eligible, underinsured, uninsured, and American Indian/Alaskan Native children.
- Promote the Iowa Care for Yourself program which provides free or low-cost breast cancer screenings (such as clinical breast exams and mammograms) and cervical cancer screenings (like Pap testing and Human Papillomavirus [HPV] testing) for Iowans between 21 and 64 years of age. *certain income requirements may determine eligibility, but the program can make recommendations for individuals who are not able to participate in the program.
- Sustain Federally Qualified Health Centers (FQHCs), Rural Health Clinics (RHCs), and Indian Health Service Health Facilities by expanding capacity and funding support.
- Support certification of Federally Qualified Health Centers (FQHCs).
- Maintain funding for state and federal programs which provide health care access to people who are uninsured or underserved.
- Establish a plan to provide equitable access to health services for those under- and uninsured during public health emergencies.
- Work with Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) to promote cancer control activities.
Strategy C: Increase patient access to health services.
Action Steps:
- Educate policymakers on evidence-based policies that increase access to health services for under- and uninsured.
- Provide community opportunities to access low-cost or free early detection cancer screenings.
- Provide transportation services and support for patients to access safety-net health services and providers, especially in urban and rural areas of the state.
- Establish and maintain health services and cancer care within the community (when possible) to minimize travel and barriers to access.
- Extend clinic hours as needed to meet the needs of individuals who do not have paid-time off from their employer.
- Educate policymakers on the need for universal access to broadband for patients to participate in telehealth services.
Strategy D: Inform policymakers on key insurance issues impacting cancer control.
Action Steps:
- Define the essential health benefits that qualified health plans must provide and ensure that these benefits affordably align with the needs of Iowans.
- Close insurance loopholes limiting an individual’s ability to obtain medically necessary prevention, genetic counseling, screening, treatment, and survivorship services.
- Ensure protection for pre-existing conditions are maintained.
- Ensure protections against lifetime limits are maintained.
- Support insurance coverage and reimbursement of patient navigators, community health workers, and other support services.
- Increase the portability of insurance coverage to eliminate gaps in coverage due to transitions in employment or life circumstances.
Data Targets
Priority 3: Prioritize health improvement approaches which engage, center, and benefit populations and communities at highest risk of health-related inequities.
Strategy A: Collect, examine, and share data on cancer health disparities.
Action Steps:
- Engage members from underrepresented communities to lead or advise on health data collection and sharing.
- Track populations through existing data collections with the highest cancer morbidity and mortality rates based on factors such as income, race, ethnicity, primary language, geography, and other social characteristics.
- Broaden existing databases and tracking systems to include the social determinants of health or other metrics to identify health inequities.
- Prioritize sharing health and cancer data with the community (e.g. press release, community forum, media interview, presentation, etc.).
- Assess rural-urban cancer rates in Iowa and develop rural-focused cancer control strategies in areas with high rural cancer incidence and mortality rates.
Strategy B: Increase community-based funding opportunities to address health disparities.
Action Steps:
- Broadly share funding opportunity announcements for cancer control efforts.
- Include community-based programs and coalitions in the development of funding opportunities.
- Increase community capacity to shape outcomes, identify funding opportunities, and receive funding.
- Identify and fund diverse partner organizations to conduct community-based participatory research and cancer education.
Strategy C: Develop health improvement activities alongside communities experiencing health inequities.
Action Steps:
- Increase representation and engagement of communities in the development and implementation of cancer control activities (i.e. leadership positions, sharing lived experiences, material review, etc.).
- Seek to identify and engage with populations experiencing the highest cancer morbidity and mortality rates based on factors such as income, race, ethnicity, primary language, geography, and other social characteristics.
- Value community experiences by incorporating community knowledge and best-practices into health improvement activities.
- Incorporate the social determinants of health into all cancer control research activities.
- Incorporate the social determinants of health into the framework and evaluation of cancer control activities and funded projects.
Strategy D: Utilize policy and systems-level changes to address the social determinants of health.
Action Steps:
- Encourage local health departments and hospitals to incorporate and address the social determinants of health in their local community health improvement plans.
- Establish a standard social determinants of health screening tool and build it into existing electronic health records.
- Establish a resource list of local programs to mitigate the negative impacts of the social determinants of health including, but not limited to referrals for free/low-cost transportation; payment assistance; food bank/pantry; and housing assistance programs.
- Increase awareness among the public and health providers about the social determinants of health and their influence on cancer rates.
- Encourage policymakers to adopt a “health in all policies” approach to consider how each and every policy will impact the health of Iowans.
- Support policies to invest in education and Iowa’s future workforce.
- Support policies to ensure employees are paid a living wage and have comprehensive health insurance offered by their employer, particularly for those suffering and unable to work due to a cancer diagnosis.
Data Targets
Priority 4: Optimize the cancer care and research workforce to be diverse, reflect the communities served, and meet the needs of all people with cancer and those at risk for cancer, ensuring they live longer and healthier lives.
Strategy A: Develop educational efforts and career pathways in oncology-related fields and jobs.
Action Steps:
- Support training programs and student experiences to develop future oncology professionals.
- Develop lessons for K-12 students to be exposed to careers in oncology and public health.
- Establish mentorship opportunities to match underrepresented health professionals and researchers with underrepresented students and trainees.
- Increase Iowa physician- and nursing-student exposure to the field of oncology.
- Increase health profession and research training opportunities for community members.
- Increase elementary, middle, and high-school health professional programs.
- Expand and extend the capacity for cancer research by engaging a diverse pool of talented learners and supporting their pursuit of a career in cancer research.
- Eliminate barriers and facilitate entry for individuals historically excluded from or underrepresented in the cancer research workforce.
- Develop new strategies and mechanisms to support career development paths in the life sciences industries and non-research science sectors, such as education, health policy, or health journalism.
Strategy B: Implement measures to retain Iowa’s existing oncology workforce.
Action Steps:
- Advocate for competitive employment packages to join/remain in the Iowa oncology workforce.
- Increase the number of oncology professionals who remain in or move to Iowa to practice.
- Protect the mental and physical health of the current oncology workforce.
- Support self-care practices for oncology workforce professionals, including resiliency training and physical and mental well-being.
- Support continuing education opportunities for the existing oncology workforce in Iowa to ensure Iowa practitioners offer the most up-to-date and quality service.
- Develop and support peer learning groups and communities of practice within the Iowa oncology workforce.
- Train existing mental health providers in oncology-related care.
- Recruit mental health providers with oncology experience.
- Support opportunities for navigator and community health worker reimbursement.
Strategy C: Recruit and retain a diverse oncology workforce.
Action Steps:
- Develop relationships with oncology-related professional societies.
- Expand the availability of loan forgiveness programs for underrepresented health professionals and researchers.
- Increase the number of health systems that reimburse tuition for members of the oncology workforce practicing in Iowa.
- Support professional development opportunities for underrepresented executive and mid-level leaders.
- Increase retention of underrepresented health professionals and researchers.
- Advocate for policies and laws that make Iowa an attractive place to practice medicine and oncology-related work.
- Educate the oncology workforce on policies and practices that increase diversity, access, inclusion, and equity in cancer care in Iowa.
- Increase underrepresented graduates from health profession higher education programs.
- Develop initiatives to address gaps and needs (e.g., more physician- and other clinician scientists) and increase the number and competitiveness of cancer researchers from underrepresented and underserved backgrounds.
- Conduct research to understand and address the unique needs and concerns of cancer researchers at all career stages and in all disciplines, including laboratory researchers, clinical care providers, data scientists, health economists, behavioral and social scientists, and all others who participate in cancer research.
Strategy D: Recruit and retain specialists, especially in areas where there is a shortage.
Action Steps:
- Increase the number of qualified palliative care providers.
- Promote palliative care rotations with physicians in training and non-physicians, such as nurse practitioners and physician assistants.
- Develop a robust, diverse, well-trained, sustainable hospice and palliative care workforce to ensure access to consistent, high-quality, equitable care for the expanding and diverse population of patients with multiple chronic conditions or life-threatening or serious illness, as well as their families and caregivers.
- Establish and support incentive programs that address LGBTQ+ health care provider shortages.
- Increase the number of palliative care fellows.
- Train community health workers or non-clinical patient navigators within communities disproportionately affected by cancer.
- Expand workforce training in childhood cancer palliative care and pediatric oncology nursing (source).
Chapter 2
Prevention and Risk Reduction
Chapter 2 Overview
Select a priority to learn more
- Priority 1 Reduce exposure to tobacco and secondhand smoke.
- Priority 2 Enhance opportunities for Iowans to access nutritious food and be physically active.
- Priority 3 Decrease alcohol consumption.
- Priority 4 Increase immunization rates for vaccines shown to reduce the risk of cancer and protect cancer patients from preventable diseases.
- Priority 5 Prevent, diagnose, and treat hepatitis C virus (HCV).
- Priority 6 Reduce exposure to environmental carcinogens.
- Priority 7 Decrease exposure to radon.
- Priority 8 Reduce exposure to ultraviolet (UV) radiation from the sun and indoor tanning devices.
Eliminate preventable cancers.
While some risk factors such as age or genetic risk cannot be changed, other risk factors such as health behaviors can be modified to lower risk and prevent disease. These include maintaining a healthy lifestyle, avoiding exposure to known cancer-causing substances, and taking medicines or receiving vaccines to prevent cancer from occuring3.
It’s estimated that in the United States, four out of every ten cancer cases are associated with preventable risk factors (source). Tobacco use is the leading cause of preventable death.
Personal health behaviors are strongly influenced by the environments in which we live, work, learn, and play. Environments that support health are those that include strong clean air laws; limited alcohol outlet density; access to safe green space; access to healthy food that is affordable and culturally appropriate; access to affordable preventive health care services; radon testing in homes and schools; workplace safety protections, and other structural factors that contribute to the personal health behaviors affecting cancer risk. While some risk factors for cancer may be avoided, many are not always within the control of an individual such as:
- High-levels of radon within an apartment complex or school;
- The tobacco industry uses tailored marketing and advertising to target some groups and communities (source).
- Occupational hazards (i.e. UV rays, agricultural chemicals, asbestos, toxic waste sites, disrupted circadian rhythms from working at night, etc.).
- Casino workers exposed to secondhand smoke.
Stories from the Iowa Cancer Plan
Priority 1: Reduce exposure to tobacco and secondhand smoke.
Note: Within this section, “commercial tobacco” refers to harmful products which are made and sold by tobacco companies. It does not include “traditional tobacco” used by Indigenous groups for religious or ceremonial purposes.
Strategy A: Prevent initiation of tobacco and nicotine use, especially among youth and young adults.
Action Steps:
- Increase the percentage of middle and high school youth receiving information to discourage the use of all tobacco/nicotine products and encourage use of cessation programs.
- Promote free trainings for retailers regarding Iowa’s tobacco sales law to increase compliance with underage buying attempts (source).
- Educate the general public (parents, teachers, students, local leaders) on the dangers of cigarettes, other commercial tobacco products, and e-cigarettes (source).
- Increase the cigarette tax.
- Support policies that tax all tobacco/nicotine products at the same rate (source).
- Increase policies to restrict youth access and use of cigarettes, other commercial tobacco products, and e-cigarettes.
- Maintain the comprehensive statewide tobacco control program and restore funding to the Centers for Disease Control and Prevention (CDC) recommended levels ($30.1 million for Iowa).
- Eliminate the sale of all flavored tobacco/nicotine products.
- Educate the public on chewing tobacco risk and providers on asking about chewing tobacco.

The Carlisle High School Iowa Students for Tobacco Education and Prevention (ISTEP) Chapter enjoy a kickoff event for the start of the year’s activities.
Strategy B: Protect and strengthen clean air laws.
Action Steps:
- Maintain and expand clean air laws and policies to include e-cigarettes (source).
- Support policies to eliminate exemptions for indoor tobacco use.
- Expand the protection of clean air laws to cover vulnerable children, including outdoor spaces and multi-unit housing (source).
- Increase the availability of smoke-free rental properties (source).
Strategy C: Increase access to and use of evidence-based nicotine addiction treatment.
Action Steps:
- Promote and support evidence-based cessation resources, especially among populations targeted by commercial marketing campaigns for tobacco use and e-cigarette use/vaping including youth, women, LGBTQ+, rural communities, and racial/ethnic minority groups, particularly the Black community (reference).
- Encourage health care provider support for evidence-based cessation treatment and resources for patients, especially among behavioral health, substance abuse treatment, LGBTQ+, and oncology providers (source, source, source).
- Encourage health care provider support for recommended annual lung cancer screening using low-dose computed tomography (LDCT) in adults aged 50 to 80 years who have a 20 pack-year smoking history, currently smoke, or have quit within the past 15 years (source).
- Increase the number of Iowa health care systems with capacity to refer patients to the Iowa Quitline via their electronic health record.
- Support and protect comprehensive, evidence-based cessation insurance benefits provided by Iowa Medicaid Enterprise and private health insurance plans.
- Educate community members about available tobacco/nicotine cessation benefits through private and public insurance plans (source).
- Educate policymakers on the cost of tobacco/nicotine use and tobacco-related disparities, including losses in employee productivity due to illness and other health-related expenses (source).
- Support and promote the Iowa Quitline as a free tobacco/nicotine cessation resource, especially among populations who experience disparities.
- Establish a plan to provide equitable access to evidence-based tobacco/nicotine addiction treatment during public health emergencies (source).
Strategy D: Identify and eliminate tobacco-related disparities.
Action Steps:
- Maintain and enhance systems to collect, evaluate, analyze, and disseminate state and community-specific data on tobacco use, with a focus on health disparities.
- Integrate efforts to eliminate tobacco-related disparities across all chronic disease prevention areas and programs across the state (source).
Resources:
- Iowa Quitline: https://www.quitlineiowa.org/en-US/, phone: 1-800-QUIT-NOW
- My Life My Quit: https://www.mylifemyquit.com/
- American Cancer Society Cancer Action Network: https://www.fightcancer.org/states/iowa
- American Lung Association Lung Action Network: www.lung.org/action
- Iowa State of Tobacco Control: https://www.lung.org/research/sotc/state-grades/iowa
- www.smokefree.gov
- Tips from Former Smokers Campaign: https://www.cdc.gov/tobacco/campaign/tips/index.html
- AHRQ Clinical Practice Guideline for Treating Tobacco Use and Dependence: https://www.ahrq.gov/prevention/guidelines/tobacco/index.html
- Iowa HHS (BRFSS 2020 Survey Snapshot re: Tobacco): https://publications.iowa.gov/43526/1/iowa_brfss_2020_infographic_tobaccouse.pdf
- American Lung Association State of Tobacco Control report: https://www.lung.org/research/sotc/state-grades/iowa
Data Targets
Note about youth health data: Created in 2019, the Iowa Youth Assessment Program originally administered three surveys related to student health (Iowa Youth Risk Behavior Survey [YRBS], Iowa Youth Survey [IYS], and School Health Profiles). Together these surveys provided necessary data for state and community members and partners to make data-driven funding, policy and program decisions. Iowa will no longer participate in the YRBS and School Health Profiles and will instead participate in the IYS (beginning 2024). Data are used at the school, county, state, and national levels to inform policy and funding, to develop program strategy, and for surveillance and research purposes.
Priority 2: Enhance opportunities for Iowans to access nutritious food and be physically active.
Note: While the terms “obesity” and “obese” are commonly used in medical and public health data, the Iowa Cancer Consortium recognizes that the terms may be stigmatizing and may not be the most useful public health measure for reducing obesity and improving health (source).
Strategy A: Create environments that support physical activity.
Action Steps:
- Educate decision-makers on evidence-based policies that create built environments to encourage safe physical activity, including local transportation plans (source).
- Educate decision-makers on evidence-based policies and programs that encourage physical activity within schools and worksites.
- Engage diverse community partners to address local barriers to physical activity (source).
- Improve access to and utilization of programs and resources that encourage physical activity, especially those available through the winter months.
- Encourage health care provider support for appropriate physical activity during and after cancer treatment.
Strategy B: Create environments that support healthy eating.
Action Steps:
- Educate decision-makers on evidence-based policies to increase the availability and affordability of local foods by connecting local farms to area workplaces, childcare, and school settings, particularly in rural and underserved communities (source).
- Educate decision-makers about food insecurity, especially among cancer patients and survivors.
- Provide incentives to establish and maintain access to supermarkets, gardens, and farmers’ markets in underserved areas, including the Double-Up Food Bucks Program.
- Engage populations experiencing health inequities in community food assessments, community health needs assessments, and other efforts to address food access (source).
- Ensure those selected for food policy councils and other food initiatives designed to improve the food environment have an understanding and the capacity to address health disparities affecting certain population groups (source).
- Educate decision-makers on evidence-based policies and programs which protect, promote and support breastfeeding-friendly environments.
- Educate decision-makers on evidence-based policies and programs that emphasize the importance of healthy eating during and after cancer treatment (source).
- In rural areas, and for communities with limited mobility (e.g. the elderly, people with disabilities), consider offering vanpools or shuttles to healthy food options (source).
- Increase connectivity between transit and healthy food retail by assessing and improving existing routes (source).
Strategy C: Identify strategies to improve accessibility, comfort and inclusion for patients in all bodies within all aspects of public health.
Action Steps:
- Encourage health care provider support to recognize and remedy examples of weight bias and weight stigma in health settings, including clinics and within cancer research.
- Educate health providers and graduate students in healthcare about the negative impacts associated with weight bias/stigma and patient care (source).
- Develop evidence-based communications on cancer risk free from weight bias/stigma and inclusive of all body types.
- Identify affirming strategies to improve accessibility, comfort, and inclusion for patients in all bodies within all aspects of healthcare and public health (source).
- Educate healthcare providers on the multifactorial causes of obesity, the impact of weight bias on a patients’ emotional and physical health, and provide training on providing compassionate care for people regarding their weight (source).
- Promote and support primary care practices to screen patients on their nutritional and physical activity needs and make appropriate referrals to community-based resources.
- Educate health providers and patients about health promoting behaviors, including the role of nutrition and physical activity as part of their cancer prevention, treatment and survivorship journey.
Resources:
- Iowa’s Supplemental Assistance Nutrition Program (SNAP): https://hhs.iowa.gov/programs/food-assistance/snap
- Iowa Healthiest State Initiative: Double-up Food Bucks Program: http://www.iowahealthieststate.com/resources/communities/double-up-food-bucks/
- Iowa Switch Program: https://www.iowaswitch.org/
- Iowa Food Bank Association: https://www.iowafba.org/
Data Targets
Priority 3: Decrease alcohol consumption.
Strategy A: Educate the public on the association between alcohol and cancer.
Action Steps:
- Educate the public on the association between alcohol and cancer (source).
- Promote health care provider education and training on how excessive alcohol use disproportionately impacts certain populations, and is a risk factor for cancer and other chronic conditions later in life.
- Educate decision-makers on communities who experience disparities from alcohol-related harms including individuals with lower socioeconomic status (SES), LGBTQ+youth, women, and racial/ethnic minorities.
- Encourage collaboration with other chronic disease programs to promote awareness of alcohol use as a risk factor for cancer.
- Identify areas of needed research regarding the relationship between alcohol use and cancer risk and outcomes (source).
- Provide education to oncology providers about the influence of excessive alcohol use on cancer risks and treatment complications, including clarification of conflicting evidence (source).
Strategy B: Create community environments that prevent and reduce the excessive use of alcohol.
Action Steps:
- Increase the alcohol tax (source & source).
- Educate decision-makers on evidence-based policies to reduce excessive alcohol use through licensing, zoning, and development practices.
- Increase local policies that limit the availability of alcohol in public spaces (source).
- Encourage and support alcohol-free and recovery friendly public environments, events, parks, and venues.
- Support state and community efforts to prevent underage drinking, including the maintenance and enforcement of Iowa social host laws; the enforcement of laws prohibiting sales to those underage; local efforts to reduce youth exposure to alcohol advertising; and alcohol education to students in Iowa’s schools (source, source , source, source).
- Support workplace policies to prevent and reduce excessive drinking (source).
- Limit the number and location of alcohol outlets by population size (source & source)
- Support and strengthen compliance monitoring and public health surveillance.
- Support additional research on alcohol-related harms and treatment for racial/ethnic and gender minorities in Iowa.
- Discourage the use of “pinkwashing” from the marketing of alcoholic beverages (e.g. using the color pink or pink ribbons to show commitment to finding a cure for breast cancer) (source).
Strategy C: Increase screening and treatment for excessive alcohol use.
Action Steps:
- Train health care providers on how to screen and provide brief interventions to patients for excessive alcohol consumption.
- Promote existing community resources that address excessive alcohol consumption.
- Educate providers and patients about addiction treatment insurance benefits.
- Promote the use of electronic screening and brief intervention (e-SBI) to facilitate the delivery of personalized feedback about the risks and consequences of excessive drinking.
Resources:
- Your Life Iowa: https://yourlifeiowa.org/
- Addressing Alcohol-Involved Deaths in Iowa (Iowa HHS, 2021): https://hhs.iowa.gov/media/11098/download?inline=
- Geospatial Analysis of Health, Safety and Tobacco Outlets in Iowa (ISU, 2021): https://faculty.sites.iastate.edu/sdorius/files/inline-files/AlcoholOutletDensities_ExecutiveReport_2021.pdf
- Centers for Disease Control and Prevention: https://www.cdc.gov/alcohol/index.htm
Data Targets
Priority 4: Increase immunization rates for vaccines shown to reduce the risk of cancer and protect cancer patients from preventable diseases.
Strategy A: Increase public awareness and knowledge of vaccines proven to reduce the risk of cancer and protect cancer patients from vaccine preventable diseases.
Action Steps:
- Create culturally relevant and accessible education campaigns to inform the public on the value of the HPV and Hepatitis vaccines as a tool for cancer prevention.
- Work with local and state immunization coalitions to disseminate information about cancer prevention vaccines to their communities (source).
- Identify communities that have lower vaccination uptake for cancer prevention vaccines and work with the community to provide education and connection to health providers.
- Educate decision-makers on the purpose of cancer prevention vaccines.
- Educate decision-makers on the underutilization of cancer prevention vaccines.
- Educate decision-makers about the safety of cancer prevention vaccines and their role in cancer prevention.
- Ensure key decision-makers and policymakers receive accurate and timely information on vaccines and strategies to promote vaccine uptake (source).
- Work with community partners to provide vaccine education to expectant/new parents on the hepatitis B vaccine.
- Share immunization rates regularly with stakeholders.
- Use evidence-based strategies to counter vaccine misinformation and disinformation and increase public support for the individual and societal benefits of vaccination, especially for protecting patients undergoing active cancer treatment (source).
- Encourage the use of diverse personal stories and community voices to reduce stigma around cancer prevention vaccines (source).
- Engage faith-based communities in education and messaging opportunities about cancer prevention vaccines (source).
- Oppose policies that would limit or restrict access to a cancer-reducing vaccine, such as the HPV vaccine.
- Educate parents, medical providers, and policymakers on the increasing incidence of oropharyngeal cancer and HPV vaccination as a solution for rising cancer rates (source).
Strategy B: Increase access to vaccination services.
Action Steps:
- Increase the availability of extended clinic hours for vaccination opportunities (source).
- Promote public-private partnerships to enhance access to vaccination services through home visits, cost reductions and vaccination programs in nontraditional settings (source, source).
- Enable pharmacists to expand their scope of practice to administer more vaccines (source).
- Collaborate with school- and university-based clinics to offer the HPV vaccine.
- Promote Vaccines for Children (VFC) federal entitlement program which provides vaccines at no cost for children whose families are uninsured or underinsured, children eligible for Medicaid, and American Indian/Alaska Native children (source).
- Increase funding for local health departments to administer cancer prevention vaccines (source).
- Identify and address disparities related to vaccine uptake and completion including financial and systems barriers (source).
- Educate partners on financial resources available for uninsured and underinsured populations for the HPV vaccine, including the Vaccines for Children Program (VFC) for pediatric populations.
Strategy C: Reduce missed clinical opportunities to recommend and administer vaccinations.
Action Steps:
- Train health care providers to review patient vaccine history and administer age-appropriate cancer prevention vaccines due at each medical encounter.
- Identify patients with incomplete cancer prevention vaccine series but still within the recommended age group and encourage completion of the vaccine series.
- Implement different methods (phone, text, email) to remind patients and caregivers to receive cancer prevention vaccines and follow-up doses (source, source).
- Create tailored interventions that reduce missed opportunities in populations with the lowest vaccine uptake.
- Encourage, train, and increase capacity for health professionals to provide strong recommendations on the benefits of vaccines that prevent cancers (source, source).
- Encourage providers to engage in shared decision-making conversations for patients aged 27-45 who might benefit from the HPV vaccine.
- Educate providers and health systems on the importance of starting the HPV vaccination at age 9.
- Encourage birthing hospitals and centers to complete universal hepatitis B vaccination within 24 hours of birth, followed by completion of the vaccine series based on Advisory Committee on Immunization Practices (ACIP) recommendations.
- Administer hepatitis B vaccine and hepatitis B immune globulin (HBIG) for infants born to hepatitis B surface antigen positive women within 12 hours of birth to prevent infection.
- Encourage birthing hospitals to enroll in the VFC Program’s birth dose hepatitis b vaccine initiative.
Strategy D: Improve statewide data reporting systems for vaccines that prevent cancers.
Action Steps:
- Maintain and promote the statewide publicly reported cancer prevention vaccine rates.
- Encourage all vaccine administrators and providers to use the Iowa Immunization Registry System (IRIS).
- Strengthen data infrastructure, including Immunization Registry Information System (IRIS), to track vaccine administration.
Resources:
- Vaccines: National Strategic Plan 2021-2025; Department of Health & Human Services: https://www.hhs.gov/sites/default/files/HHS-Vaccines-Report.pdf
- Vaccines for Children (VFC): https://idph.iowa.gov/immtb/immunization/vfc
- Iowa Immunizes: https://www.iowaimmunizes.org/
- Iowa Public Health Association: https://iowapha.org/
- American Academy of Pediatrics (Iowa): http://www.iowapeds.org/
- Iowa Public Health Tracking Portal: https://tracking.idph.iowa.gov/Health/Immunization
Data Targets
Priority 5: Prevent, diagnose, and treat hepatitis C virus (HCV).
Strategy A: Increase education and awareness of the relationship between hepatitis C and cancer.
Action Steps:
- Educate health providers, patients, and their families about hepatitis C and testing recommendations (source).
- Encourage health systems to utilize evidence-based strategies, such as system-based patient reminder tools, to identify patients recommended for HCV testing.
- Educate policy makers on evidence-based interventions, such as Syringe Services programs (SSPs) to prevent transmission of HCV.
- Increase the number of people with chronic HCV who receive and complete treatment, especially among individuals who use drugs and people in correctional settings (source).
- Reduce barriers to accessing treatment for HCV for both private and public insurance providers, including coverage, cost, and prior authorization requirements (source).
Strategy B: Increase the proportion of people who are tested and aware of their HCV status and receive treatment.
Action Steps:
- Support and promote free or low-cost HCV testing, especially for people who are uninsured or underinsured.
- Expand routine/opt-out HCV testing in clinics, health systems, and emergency departments.
Resources:
- Viral Hepatitis Nation Strategic Plan 2021-2025: https://www.hhs.gov/sites/default/files/Viral-Hepatitis-National-Strategic-Plan-2021-2025.pdf
- Iowa HHS, Hepatitis C Program: https://hhs.iowa.gov/public-health/data/health/hepatitis-c
- Stop Hepatitis Iowa: https://www.stophepatitisiowa.org/
Data Targets:
As of 1/22/2023, Hepatitis C data will be forthcoming and posted as soon as it is available.
Priority 6: Reduce exposure to environmental carcinogens.
Strategy A: Increase awareness of the connection between environmental carcinogens and cancer risk.
Action Steps:
- Educate the public, health care providers, public health officials, schools, property owners, property managers, and policymakers about the link between environmental carcinogens of concern in Iowa and negative health impacts, specifically polyfluoroalkyl substances (PFAS); arsenic; and nitrates.
- Develop an awareness campaign about the sources of and routes of exposure to carcinogens in the environment and how reducing exposure can prevent disease.
- Develop an awareness campaign about environmental carcinogens.
Strategy B: Reduce occupational exposures to known carcinogens.
Action Steps:
- Tailor outreach and awareness efforts for occupational exposure to carcinogens (e.g. educate firefighters on their increased risk for digestive, oral, respiratory [mesothelioma], and urinary cancers).
- Raise awareness on and educate agricultural workers on the link between certain agricultural practices and pesticide use, and cancer.
- Educate employers and workers on the importance of personal exposure monitoring and appropriate use of personal protective equipment, to reduce occupational exposure to asbestos and other known carcinogens.
Strategy C: Reduce exposure to known and probable environmental carcinogens and investigate not yet identified sources of exposure.
Action Steps:
- Educate public health officials and health care providers about provider practice interventions and health systems support related to known, suspected, and emerging environmental carcinogens.
- Support continued education on the importance of the proper management of wastewater, solid and hazardous waste, and control of toxic substances to prevent public exposure to carcinogens.
- Work with the Zoning sector to ensure safe siting of homes, schools, parks, and community centers in or around industry or where industry used to be to limit environmental exposure risks (i.e. brownfield sites, contaminated sites), especially those environments created by both social and environmental injustices that lead to health disparities, including red lining and zoning policy.
- Advocate for additional state funding for water testing that does not compete with existing funds for testing, remediation, and closing of private wells.
- Support initiatives to reduce chemicals/pollutants and known and/or probable carcinogens in drinking water, recreational water, air, and wastewater.
- Work with partners including the Iowa Department of Transportation and local public health agencies to reduce the incidence and prevalence of lung cancer and respiratory diseases associated with exposure to fine particulate matter air pollution, ozone, pollen/allergens, molds and indoor moisture levels, by improving (indoor and outdoor) air quality across Iowa.
Strategy D: Address and mitigate exposures among specific groups put at a higher risk such as children, expectant and birthing individuals, low socioeconomic status populations, communities of color, immigrants, occupational workers including farm workers, cancer survivors in remission, and others.
Action Steps:
- Advocate for the reduction, restriction, and elimination of the use of known carcinogens in and around public spaces, prioritizing locations that prevent early-life exposure.
- Collaborate with public health officials and health care providers to provide educational materials to expectant and birthing individuals, parents, or caregivers on mitigating risk to environmental carcinogens.
- Require cumulative environment impact assessments before permitting additional polluting industries in environmentally overburdened communities.
Strategy E: Support research that further identifies chemicals and other environmental factors involved in cancer development and primary prevention strategies to reduce exposure.
Action Steps:
- Compile an inventory of known, probable, and suspected carcinogens in Iowa (source), including potential routes of exposure and susceptible/at-risk population groups.
- Support environmental monitoring for chemicals/pollutants and known and/or probable carcinogens in drinking water, recreational water, air, and wastewater.
- Support a research and innovation agenda for development of safe and sustainable alternatives to hazardous chemicals.
- Support interdisciplinary spatial life course epidemiological initiatives and research focused on evidence-based epidemiologic and environmental monitoring of carcinogen exposure, including multigenerational exposures.
Strategy F: Identify high priority environmental hazards and preventive actions families and communities can take.
Action Steps:
- Support and advocate for renewable energy to reduce hazardous air pollution linked to lung and other cancers.
- Prevent potential exposures to toxic chemicals and raw sewage that may result from more frequent heavy rain/flooding events.
- Identify and address decreased water quality resulting from elevated water temperatures and already high nutrient levels (i.e., harmful algae blooms).
- Advocate for Polluter Pays laws relating to both clean up, monitoring, and treatment costs.
- Develop partnerships with community organizations working on environmental health issues in Iowa to address the overlap of environment and cancer, such as the Iowa Citizens for Community Improvement, Des Moines Waterworks, Iowa Environmental Council, Iowa Environmental Health Association, Iowa Public Health Association, Iowa agricultural organizations, One Thousand Friends of Iowa, Iowa Department of Natural Resources, State Hygienic Lab, allied health professions associations in Iowa, Iowa Occupational Safety and Health Administration, Proteus Inc., Iowa Farmers Union, Iowa Department of Agriculture and Land Stewardship, Iowa Chapter of Physicians for Social Responsibility.
Resources:
- How to test your private well: IDNR, Private well testing FAQ; Information on free private well testing: Grants to Counties
- Iowa Environmental Tracking Portal
- Ways to identify harmful chemicals and carcinogens in household, cleaning, and personal care products:
- Silent Spring Institute: Detox Me app
- Clearya app and browser extension
- Environmental Working Group’s Skin Deep Database and App
- Paths to Prevention: California Breast Cancer Primary Prevention Plan – Breast Cancer Prevention Partners (BCPP)
- Breast Cancer Action: The Climate Crisis and Breast Cancer
- American Lung Association State of the Air report: https://www.lung.org/research/sota/city-rankings/states/iowa
- EPA’s Tri Toxics Tracker
- Iowa Department of Natural Resources’ Greenhouse Gas Emission Inventory Report
- Farming For Public Health https://farmingforpublichealth.org
- Good Neighbor Iowa https://goodneighboriowa.org
Data Targets
Priority 7: Decrease exposure to radon.
Strategy A: Increase awareness and research around the connection between radon and cancer risk.
Action Steps:
- Educate the public, health care providers, public health officials, school administrators, property owners, property managers and policymakers about radon and its link to lung cancer.
- Encourage home builders and realtors to educate clients regarding radon, cancer risk, testing, and mitigation.
- Support research and funding to increase the evidence for radon-related cancer risks.
- Support research and funding to increase knowledge about the effects of climate change on radon levels.
- Enhance data collection to understand the impact of radon in different geographic and socioeconomic areas of the state.
- Promote continued research between the synergistic effect of radon, tobacco use, and secondhand smoke.
Strategy B: Increase the testing for and mitigation of radon in homes and other buildings.
Action Steps:
- Increase the percentage of Iowans who test their homes for radon and mitigate when needed.
- Increase the number of residential properties/units in low-income neighborhoods that test for radon and install radon mitigation equipment when indicated.
- Collaborate with cities, housing departments, and other organizations to develop initiatives that provide financial assistance for radon testing and mitigation.
- Require radon testing and mitigation in multi-housing units and rental housing.
- Support policies to require radon notification and disclosure during the real estate leasing transaction.
- Support efforts to implement the Gail Orcutt School Radon Safety Act requiring radon testing and mitigation in Iowa public schools (HF2412).
- Encourage development and dissemination of information regarding radon policies and education to radon professionals.
Strategy C: Increase the number of residential and other buildings built or remodeled using radon reducing methods.
Action Steps:
- Require newly constructed homes and buildings to be built using passive radon control methods according to the 2015 International Residential Building Code.
- Support workforce development for radon testing and mitigation professionals, especially for large buildings.
Resources:
- The National Radon Action Plan 2021-2025: https://www.epa.gov/radon/national-radon-action-plan-strategy-saving-lives
- Iowa HHS (Radon Program): https://hhs.iowa.gov/public-health/radiological-health/radon
- Iowa Radon Hotline: https://www.lung.org/clean-air/at-home/indoor-air-pollutants/radon
Data Targets
Priority 8: Reduce exposure to ultraviolet (UV) radiation from the sun and indoor tanning devices.
Strategy A: Increase opportunities for sun protection in outdoor settings.
Action Steps:
- Increase availability and use of shade structures in outdoor settings, including schools, worksites, and recreational sites.
- Educate decision-makers about evidence-based policies to reduce exposure to UV radiation including use of shade structures and providing SPF 15 or higher sunscreen in both public and private spaces.
- Implement evidence-based school, worksite and community sun safety programs.
- Increase availability and use of shade structures and sunscreen in low-income communities.
Strategy B: Increase awareness about skin cancer prevention and screening.
Action Steps:
- Encourage health care providers to educate patients about skin protective behaviors, including patients with darker complexions to normalize skin protective behaviors.
- Educate health care providers on diagnosing skin cancer in people of color at an early-stage, when the cancer is most treatable.
- Provide tailored skin cancer education for Iowans who work outside.
- Collaborate with state and local parks and the Iowa Department of Natural Resources to promote sun-safety.
- Support initiatives that promote diversity in dermatological education such as ensuring skin of color is featured in dermatology textbooks.
- Educate health care providers about risk factors and symptoms of skin cancer in skin of color.
Strategy C: Decrease indoor tanning use.
Action Steps:
- Educate the public and policymakers on evidence-based policies that reduce indoor tanning use, especially among youth.
- Reduce access to indoor tanning for minors under the age of 18.
- Develop a public awareness campaign to highlight the dangers of indoor tanning.
Strategy D: Enhance research support for skin cancer and melanoma.
Action Steps:
- To account for the diverse lived experiences and exposures of various populations, clinical trials must be appropriately inclusive of racial and ethnic minority groups, as well as other populations experiencing health disparities, including sexual and gender minority or socioeconomically disadvantaged populations.
- Continue financial support of melanoma research efforts at the national and state-level.
- Skin of Color Society: https://skinofcolorsociety.org/patient-dermatology-education/sun-protection-for-skin-of-color/
- Blogpost: Sun-Safety for Skin of Color https://canceriowa.org/sun-safety-for-skin-of-color/
- https://jamanetwork.com/journals/jamadermatology/fullarticle/2774110
- https://www.aad.org/public/diseases/skin-cancer/types/common/melanoma/skin-color
- https://uihc.org/services/ethnic-skin-care-clinic
- https://www.npr.org/sections/codeswitch/2018/07/05/559883985/will-your-melanin-protect-you-from-the-sun
- https://melanoma.org/
- https://www.cancer.org/healthy/be-safe-in-sun.html
As of 1/22/2023, UV/Sun-Safety data will be forthcoming and posted as soon as it is available.
Chapter 3
Early Detection and Screening
Chapter 3 Overview
Select a priority to learn more
- Priority 1 Increase awareness of recommended cancer screenings.
- Priority 2 Empower health care systems to strengthen cancer screening and diagnostic services.
- Priority 3 Support strategies to increase access to cancer screening and diagnostic services.
- Priority 4 Increase access to cancer risk assessment and genetic counseling services.
- Priority 5 Enhance awareness and research support for the early detection of ovarian cancer.
- Priority 6 Support research and innovation in cancer early detection and screening.
Promote the benefits of screening tests to ensure early diagnosis.
When cancer is diagnosed early, a patient’s treatment is often more effective and longer survival is more likely. In fact, there are some cancer screening tests that have the ability to detect and remove cells that have the ability to turn into cancer (i.e. a colonoscopy allows for the removal of precancerous polyps before they ever turn into cancer).
Several cancer screening tests are considered effective and recommended by expert groups including breast, cervical, colorectal, and lung cancer screening. Unfortunately, there are cancers that do not have a specific screening test and require additional research including pancreatic and ovarian cancers.
To help inform patients and medical providers, there are a few national organizations who have created cancer screening guidelines to help patients and families make their decision:
- American Cancer Society
- United States Preventive Services Task Force (USPSTF)
- National Comprehensive Cancer Network (NCCN)
Ultimately, Iowans should work with their medical team to determine their risk for developing certain cancers and which screening methods are best for them. However, there are many things Iowans can do to encourage cancer screening rates:
- Provide opportunities for Iowans to learn about cancer screening guidelines and opportunities.
- Encourage Iowans to identify a trusted medical provider or medical “home” for their care.
- Share state and local cancer screening programs to serve uninsured or underinsured Iowans.
- Make sure cancer screening services are offered in an inclusive, supportive and safe setting.
- Ensure when screening tests detect cancer, that all patients are able to easily and readily access cancer treatment for the best outcome.
This chapter describes the individual, community, clinical, policy and systems approaches needed in Iowa to support the early-detection of cancer.
Stories from the Iowa Cancer Plan
Priority 1: Increase awareness of recommended cancer screenings.
Strategy A: Develop public awareness campaigns designed to reach communities and populations with the greatest need for cancer screening.
Action Steps:
- Create public awareness campaigns on cancer screening recommendations, including the ways a persons family cancer history may change those recommendations.
- Ensure educational materials and decision tools about recommended cancer screenings are age, literacy, and culturally appropriate for the community being served.
- Keep decision-makers informed on current recommendations for cancer screenings and areas of need.
- Partner with worksites to promote available cancer screening benefits through private insurance.
- Empower LGBTQ+ coalitions and organizations to offer tailored outreach and education on cancer screening to Iowans.
- Work alongside faith communities to educate members on the importance of cancer screening.
- Encourage insurers to promote recommended cancer screening to their members, including Iowa’s managed care organizations (MCOs).
- Engage cancer patients and survivors as champions to promote cancer screening.
- Enhance cancer education-focused community engagement to promote structural changes that increase prevention and early detection measures.
- Address the need for improving health literacy by developing culturally relevant education programs that increase community wellness.
Strategy B: Use community-based strategies to strengthen community education, trust, and utilization of cancer screening services and the healthcare system.
Action Steps:
- Develop initiatives focused on reaching specific communities and their specific screening recommendations (e.g. Black men for prostate cancer screening, cancer survivors for screening recommendations post-treatment, patients who identify as LGBTQ+ and specifically naming cancer screenings available for specific organs or areas of the body).
- Wherever possible, work with community leaders and utilize peer-to-peer educators (i.e. community health workers) to promote cancer screening information – especially amongst communities who have been marginalized or experienced racism within the health care system.
- Work with LGBTQ+ organizations to identify and reduce regional and state-specific barriers to timely cancer screening.
- Encourage all health systems to work with community organizations to distribute culturally and linguistically-appropriate patient navigation systems to increase uptake of cancer screenings.
- Identify, recognize, and support local physicians, public health organizations, and clinics who promote cancer screening.
Strategy C: Use data to identify gaps in access, cost and quality for patients.
Action Steps:
- Work with organizations like the Iowa Cancer Registry and Iowa Department of Health and Human Services (Iowa HHS) to monitor cancer disparities data.
- Coordinate with the Iowa Cancer Registry to actively review late-stage cancer
- Coordinate with government agencies and the Iowa Cancer Registry to relay local surveillance of cancer disparities among vulnerable populations (e.g. by county, race, ethnicity, geography, income, education level, and disability status).
- Identify data sources and assist stakeholders in understanding and using key data to identify priority populations, including addressing pandemic-related disruptions exacerbating existing disparities in cancer screening.
Resources:
- American Cancer Society: Cancer Screening Guidelines by Age https://www.cancer.org/healthy/find-cancer-early/screening-recommendations-by-age.html
- Centers for Disease Control and Prevention, Cancer Screening Tests https://www.cdc.gov/cancer/prevention/screening.html
- The Community Guide: Cancer https://www.thecommunityguide.org/topic/cancer
Data Targets
Priority 2: Empower health care systems to strengthen cancer screening and diagnostic services.
Strategy A: Encourage health systems to identify or develop quality improvement metrics and processes to improve cancer screening rates and diagnostic care.
Action Steps:
- Develop quality improvement metrics to improve cancer screening rates and timely diagnostic referral.
- Foster a clinic environment which includes tracking and sharing of quality improvement goals and celebrating successes.
- Identify, recognize, and support local physicians, public health organizations, and clinics who promote cancer screening.
- Wherever possible, encourage providers and health systems to utilize evidence-based strategies to increase cancer screening rates (i.e. client reminders and group education for breast cancer).
- Create a quality improvement team focused on patient population groups with the lowest cancer screening rates.
- Work to reduce the time between an initial cancer screening and follow-up diagnostic services for individuals whose results may indicate cancer.
- Set goals to reduce the time between a patient’s official cancer diagnosis to their first treatment.
Strategy B: Encourage providers to utilize shared-decision making to address patient needs.
Action Steps:
- Utilize patient decision tools which incorporate family history, previous cancer screening, and behavioral risks into screening recommendations.
- Eliminate discriminatory exclusion practices for LGBTQ+ patients specifically related to recommended cancer screening and perceived discordance between their gender markers and anatomy.
Strategy C: Create opportunities and tools for providers to remain up-to-date on current cancer screening recommendations for all populations.
Action Steps:
- Whenever possible, offer free or low-cost continuing education opportunities for health care providers on the latest cancer screening recommendations, patient communication techniques, and health disparities.
- Partner with state/national medical associations highlight any changes to cancer screening recommendations for current providers.
- Provide sample language and decision aids for health providers to use when discussing screening recommendations with patients.
- Train staff at all clinic levels to provide inclusive and affirming service to LGBTQ+ patients, their family, and their chosen support person(s) throughout the cancer screening experience.
- Provide information to health care providers and patients about the availability of free and low-cost screenings and how to access them.
- Offer local primary care providers on how to correctly recognize and respond to early signs and symptoms of childhood cancers.
Strategy D: Reduce structural barriers within the health system related to cancer screening.
Action Steps:
- Provide opportunities to access low-cost or free cancer screenings and access to affordable diagnostic testing and treatment.
- Whenever possible, support existing community-based efforts to promote recommended cancer screening.
- Establish a plan to provide equitable access to cancer screening during public health emergencies.
- Create opportunities to interact with the community through cancer education and screening programs (e.g. ask the community to define barriers to screening, identify innovative community solutions, etc.).
- Encourage collaboration amongst service providers to ensure access to timely treatment and best outcomes for the patient – including working across health systems.
- Provide culturally-affirming and linguistically-appropriate patient navigation systems to increase the uptake of recommended cancer screenings (e.g. non-clinical patient navigators, community health workers, etc.).
Resources:
- United State Preventive Services Task Force (USPSTF) https://www.uspreventiveservicestaskforce.org/uspstf/
- American Cancer Society, Information for Health Care Professionals https://www.cancer.org/health-care-professionals.html
- Care for Yourself – Iowa’s Breast and Cervical Cancer Early Detection Program https://hhs.iowa.gov/public-health/cancer/cfy
- Iowa Get Screened: Colorectal Cancer Screening Program https://hhs.iowa.gov/public-health/cancer/colorectal-cancer-screening-program
- Colon Cancer Foundation of Iowa http://www.coloncanceriowa.org/
- Splash of Color https://splashofcolorbcsg.com/
- Susan G. Komen – Iowa https://www.komen.org/community/iowa/
- Iowa Army of Pink/Breast Density Iowa Army of Pink
- Cervivor: https://cervivor.org/
- CDC Resource for African American Women re: Cervical Cancer Face Your Health
- American Cancer Society, A Guide to Cervical Cancer https://www.cancer.org/cancer/cervical-cancer.html
Priority 3: Support strategies to increase access to cancer screening and diagnostic services.
Strategy A: Take steps to increase patient access to cancer screening through policy change.
Action Steps:
- Advocate for government and commercial payers to cover the cancer screening process, with no out-of-pocket burden to patients.
- Monitor the introduction and passage of state/federal policy involving cancer screening, including attempts to address loopholes in coverage and costs associated with diagnostics and follow-up care.
- Inform policymakers at all levels about the benefits of recommended cancer screening and need for accessible population health services and programs.
- Ensure Iowans are represented and aware of activities happening at the American Cancer Society’s national roundtables, including but not limited to: National Breast Cancer Roundtable, National Colorectal Cancer Roundtable, National HPV Vaccination Roundtable, National Lung Cancer Roundtable, National Navigation Roundtable, and National Roundtable on Cervical Cancer.
- Support existing free or low-cost cancer screening programs in Iowa.
- Develop research partnerships that include primary care providers, researchers, and communities at increased risk for cancer to improve the testing and adoption of effective cancer screening.
Resources:
- Care for Yourself – Iowa’s Breast and Cervical Cancer Early Detection Program https://hhs.iowa.gov/public-health/cancer/cfy
- Iowa Get Screened: Colorectal Cancer Screening Program https://hhs.iowa.gov/public-health/cancer/colorectal-cancer-screening-program
Priority 4: Increase access to cancer risk assessment and genetic counseling services.
Strategy A: Educate providers and patients about assessing genetic cancer risk.
Action Steps:
- Offer free or low-cost continuing education opportunities for health providers about genetic risk assessments and counseling – including recommending an initial cancer risk assessment and if needed, how to refer patients to a qualified cancer genetic counselor.
- Create a public education campaign focused on the role of genetic risk assessments and genetic counseling, and their important role in cancer early-detection.
- Share culturally and linguistically appropriate patient education materials on assessing genetic cancer risk.
- Encourage Iowans to know their family health history and share the information with their primary care provider.
Strategy B: Increase the availability of cancer genetic risk assessments and counseling.
Action Steps:
- Develop provider reminder systems for cancer genetic risk assessment and counseling.
- Promote the benefits of having qualified cancer genetic counselors on staff to health care systems.
- Encourage health insurance plans, including Medicaid, to cover cancer risk assessment and genetic counseling for both in-person and telehealth services.
- Utilize secure telehealth technology and services to enhance patient access to genetic counseling services, especially for patients with transportation barriers or reside in a rural location.
- Establish a preparedness plan to provide equitable access to cancer genetic risk assessment and counseling during public health emergencies.
Strategy C: Establish insurance coverage for cancer genetic risk assessment and counseling.
Action Steps:
- Educate policymakers on the need for health insurance coverage of genetic counseling and testing according to evidence-based guidelines.
- Educate policymakers on the role of state licensure in ensuring a qualified cancer genetic counselor workforce.
- Promote Advanced Genetics Nursing-Board Certified (AGN-BC) and Certified Genetic Counselor (CGC) credentialing to increase access to providers trained in cancer genetic counseling.
Strategy D: Enhance research support for genetic testing.
Action Steps:
- Support efforts to obtain federal and state research funding for cancer genetic research.
Resources:
- National Society of Genetic Counselors “Find a Genetic Counselor” (source)
- Medline Plus: Genetics (source)
- American Cancer Society: Understanding Genetic Testing for Cancer (source)
Data Targets:
As of 1/22/2023, genetic testing and counseling data will be forthcoming and posted as soon as it is available.
Priority 5: Enhance awareness and research support for the early detection of ovarian cancer.
A Note from the Iowa Cancer Consortium:
- At this time, there is no screening test for ovarian cancer. However, the Iowa Cancer Plan contains best-practice guidance for the early-detection of some ovarian cancers.
- While some of the action steps and data measures refer to “women”, the Iowa Cancer Consortium understands that not everyone with internal reproductive organs/a uterus identifies as woman or female.
Strategy A: Educate providers and patients about assessing ovarian cancer risk and early detection.
Action Steps:
- Increase patient and provider knowledge of ovarian cancer symptoms.
- Create public awareness campaigns or community education about the symptoms of ovarian cancer (e.g. abdominal pain or pressure, bloating, constipation, urinary symptoms, back pain, or fatigue).
- Encourage patients with a family history of ovarian or breast cancer to discuss their family history with their primary care provider, as they may be at risk for hereditary cancer syndrome.
- Engage ovarian cancer survivors and caregivers in provider education.
Strategy B: Increase the availability of cancer genetic risk assessments and counseling.
Action Steps:
- Expand insurance coverage of genetic counseling and testing to include provisions for risk-reducing interventions if necessary.
- Expand the Affordable Care Act’s preventive health benefit to cover genetic testing and counseling for women with a family history of breast and ovarian cancer at no out-pocket cost to the patient (going above and beyond current BRCA 1 and BRCA 2 mutation coverage).
Strategy C: Ensure access and availability to high quality treatment and care for patients with ovarian cancer.
Action Steps:
- Ensure all people with ovarian cancer receive timely standard of care treatment including access to a gynecologic oncologist for surgery; standard of care chemotherapy regimens and targeted therapies outlined by the National Comprehensive Cancer Control Network (NCCN).
- Make sure ovarian cancer patients are offered the chance to participate in clinical trials.
Strategy D: Support opportunities for ovarian cancer research.
Action Steps:
- Support public investments in ovarian cancer research, awareness, and education.
- Leverage private funding to allow researchers to pursue ovarian cancer breakthroughs.
- Support research efforts to identify better ways to screen for ovarian cancer.
- Support efforts to expand ovarian cancer clinical trials.
Resources:
- NormaLeah Ovarian Cancer Initiative: https://www.normaleah.org/
- National Ovarian Cancer Coalition: https://ovarian.org/
- Ovarian Cancer Research Alliance (ORCA): https://ocrahope.org/
- National Comprehensive Cancer Network (NCCN): https://www.nccn.org/
Priority 6: Support research and innovation in cancer early detection and screening.
Strategy A: Develop new methods to detect cancers, particularly for those cancers where no effective screening tests currently exist.
Action Steps:
- Conduct rigorous clinical trials to capture evidence about the benefits and harms of novel cancer detection tests.
- Develop methods to identify precancerous cells and eliminate them while minimizing side effects.
Chapter 4
Diagnosis and Cancer-Directed Therapy
- Overview
- Priority 1
- Priority 2
- Priority 3
- Priority 4
- Priority 5
- Priority 6
- Priority 7
- Priority 8
- Priority 9
- Priority 10
Chapter 4 Overview
Select a priority to learn more
- Priority 1 Increase access to quality, evidence-based cancer treatment and affirming care.
- Priority 2 Increase access to targeted therapy options for Iowans, including biomarker testing.
- Priority 3 Enhance patient support services within the clinic.
- Priority 4 Empower patients and providers to communicate about advance care planning early in the cancer treatment journey.
- Priority 5 Increase patient and caregiver access to non-clinical support services.
- Priority 6 Enhance awareness of and participation in cancer research of all types, and accelerate scientific findings into policy and practice.
- Priority 7 Ensure early access to palliative care.
- Priority 8 Provide high-quality childhood cancer care.
- Priority 9 Provide high-quality adolescent and young adult (AYA) oncology care.
- Priority 10 Ensure patients undergoing treatment are prepared for a natural disaster and/or emergency.
Reduce barriers to care, promote evidence-based practices, and encourage participation in clinical trials.
When cancer is found, an individual’s survival and quality of life can depend on the availability of timely, quality treatment. The Institute of Medicine have identified six components of high-quality cancer care, including the following:
- A system that supports all patients to make informed decisions about their care.
- A well-staffed, trained and coordinated workforce.
- A system that uses scientific research to inform medical decisions.
- A system that uses advances in information technology to enhance quality and care delivery.
- A system that translates evidence into clinical practice, quality measurement and performance improvement.
- A system that is accessible to all and uses new payment models to reward quality care and eliminate waste.
Yet, Iowans face a number of common barriers to accessing lifesaving cancer treatment, including:
- Lack of, or inadequate, health insurance coverage (including high deductibles or copayments).
- Limited availability of oncology specialists or treatment centers.
- Inadequate information and guidance for patients about treatment options and quality of care.
- Access to adequate health insurance.
- Transportation to medical facilities where quality care is available, especially in rural parts of the state.
- Financial insecurity.
- Barriers related to culture, language and/or identity.
- Competing basic needs and priorities.
- Overall availability of a qualified cancer workforce.
- Lack of awareness or understanding of the benefits of clinical trials.
Additionally, cancer research at all phases – including clinical trials – must be adequately supported so that new, emerging and more effective treatment methods are developed and utilized. And, quality of life interventions such as physical activity and nutrition programs can enhance and should be considered a crucial part of cancer treatment.
This plan addresses identified barriers to quality cancer treatment at the community and system levels, and recognizes the wide range of partners who must work collaboratively on a comprehensive approach to caring for Iowans.
Stories from the Iowa Cancer Plan
Priority 1: Increase access to quality, evidence-based cancer treatment and affirming care.
Strategy A: Reduce time between diagnosis and treatment.
Action Steps:
- Streamline coordination of care between health facilities and systems as the patient with cancer moves from screening to treatment.
- Reduce barriers within the healthcare system, such as insurance prior authorization requirements that prevent providers from recommending treatments, timely imaging, genetic and molecular lab testing, and other lab/radiology procedures.
- Implement quality improvement (QI) projects to reduce the time between diagnosis and treatment.
Strategy B: Increase access to cancer treatment.
Action Steps:
- Create and maintain high-quality community engagement programs to establish relationships between community members and cancer treatment facilities.
- Utilize secure telehealth technology and services to increase access to care (source).
- Create and provide resources and information for all patient languages, including translators, interpreters, and the use of translation technology when needed (source).
- Support the implementation of evidence-based policy and systems change to reduce transportation-related barriers in receiving recommended cancer treatments (source).
- Support initiatives that address patient adherence to their cancer treatment plan, including offering treatment close to home (when possible).
- Establish a plan to provide equitable access to cancer treatment during public health emergencies (source).
- Develop approaches that maximize equitable access to proven treatments (source).
- Assist parents of children without health insurance to apply for insurance (source).
Strategy C: Ensure adherence to treatment guidelines and quality care standards.
Action Steps:
- Increase the number of cancer patient care facilities in Iowa participating in quality improvement programs, such as the American College of Surgeons’ Commission on Cancer® (CoC) accreditation program and/or the American Society of Clinical Oncology (ASCO) Quality Oncology Practice Initiative (QOPI®) certification program.
- Support policies that address systemic deficiencies in the law, regulation, and science policy that result in the approval of drugs that do not significantly extend or save lives and whose prices are not based on value or effectiveness (source, source).
- In the absence of LGBT-specific treatment guidelines, follow standard of care/current treatment data to meet the standard of care (source).
- Maintain appropriate hormone regimens and transition-related services for transgender and gender variant patients during cancer treatment as a standard of care, in the absence of compelling data to the contrary (source).
- Develop approaches that minimize toxicities from cancer treatment and that detect and lessen short- and long-term effects of treatment, including secondary cancers in cancer survivors (source).
Strategy D: Create welcoming and affirming environments for cancer care.
Action Steps:
- Ensure nondiscrimination on the basis of sexual orientation and gender identity in hospital visitation, surrogate medical decision making, etc. according to Centers for Medicare & Medicaid Services and Joint Commission Accrediting Standards (source).
- Increase the availability and utilization of culturally affirming, linguistically diverse, and low-literacy cancer diagnosis and treatment information materials.
- Provide gender neutral diagnostic facilities and programs for all cancers, including cancers traditionally treated in gender-specific facilities (source).
- Create and/or expand culturally affirming LGBTQ+ provider listings/registries.(source).
- Increase engagement with LGBTQ+ cancer survivors and provide training for welcoming oncology offices (source).
- Include LGBTQ+ topics in all cultural competence training across the health care treatment workforce (including clerical, technicians, patient navigator, pharmacy, housekeeping, food service, etc.)(source).
- Recruit and train diverse patient navigators and community health workers representative of the communities they serve to guide and support patients and caregivers.
- Encourage health systems and institutions to promote available cancer information resources and utilize existing referral systems within the community.
Strategy E: Provide survivorship care plans to patients.
Action Steps:
- Upon completion of their first course of treatment, provide patients with a comprehensive care summary and follow-up care – together creating the patient’s Survivorship Care Plan (source).
- Collaborate with hospitals and other health care systems to integrate LGBTQ+ issues within survivorship care plans (source).
Data Targets
Priority 2: Increase access to targeted therapy options for Iowans, including biomarker testing.
Strategy A: Educate providers and patients about biomarker testing in cancer care.
Action Steps:
- Educate policymakers and the public about biomarker testing.
- Educate health care providers about current biomarker testing guidelines.
Strategy B: Support insurance coverage and timely access to biomarker testing.
Action Steps:
- Support coverage of National Comprehensive Cancer Network® (NCCN®) guideline-indicated biomarker testing and FDA-cleared or -approved companion and complementary diagnostics as necessary biomarker testing to evaluate patient eligibility for targeted cancer therapy (source).
- Provide coverage for multi-gene panel testing as indicated by NCCN® guidelines, when it is more efficient, when a single analyte test does not exist, or when tissue availability is too limited for use of multiple single analyte testing.
- Provide coverage for tumor-diagnostic biomarker tests as medically appropriate.
- Provide coverage and access to appropriate services for the interpretation of biomarker tests.
- Support policies to expand the availability and access to biomarker testing, including coverage across various cancer stages, retesting after a medically appropriate interval, and timely utilization review practices (prior authorization).
- Expand state Medicaid coverage to include biomarker testing.
Strategy C: Use biomarker testing in clinics for the most effective cancer treatment.
Action Steps:
- Equip providers and institutions with tools (e.g. clinical decision support), resources (e.g. access to a tumor board), and training for the efficient collection and handling of tissue for testing and for proper test selection, administration, and interpretation.
- Promote adoption and utilization of clinical decision support tools for biomarker testing that incorporate evidence-based clinical guidelines at the point of care to guide testing and treatment decisions.
- Facilitate use of newly discovered biomarkers that improve patient outcomes into standard practice.
- Make the fullest possible use of available resources to identify biologically informed therapeutic targets (source).
Strategy D: Support continued research for precision medicine in cancer treatment.
Action Steps:
- Encourage providers to use results from biomarker testing to inform patients of relevant clinical trial opportunities.
- Promote use of biomarkers for population research and surveillance.
- Develop effective methods for predicting if patients will respond to treatment and their likely long-term outcomes (source).
Resources:
Priority 3: Enhance patient support services within the clinic.
Strategy A: Streamline and increase accessibility of clinical support services.
Action Steps:
- Adopt distress/symptom assessment tools and workflow models that identify the physical, social, psychological, and spiritual needs of patients throughout their cancer treatment (source).
- Develop systems that make support services available to all cancer patients and survivors (source).
- Encourage health systems to have supportive care team members on staff to minimize referrals needed, such as patient navigators, social workers, genetic risk counselors, nutritionists, psychiatrists, and rehabilitation therapists (source).
- Identify and address gaps in access to non-clinical support services for underserved populations (source).
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Strategy B: Promote shared-decision making between patients, families, and providers about treatment options and goals of care.
Action Steps:
- Develop and disseminate culturally and linguistically appropriate materials and decision-aids for supporting conversations about goals of care.
- Employ patient navigators and community health workers to support and teach patients to be a partner in setting goals of care.
- Include long-term risks of treatment (including second cancers) in discussions before, during, and after treatment for certain cancers.
- Provide multiple opportunities for patients to discuss, establish, and maintain goals of care with their care team as their treatment progresses.
- Increase the length of appointments to allow for additional conversations between patients and providers and their care.
- Identify and address patient and family care and cancer-related educational needs such as diagnosis, treatment, fertility, late effects, psychosocial support programs, sibling support, and respite care (source).
Strategy C: Address fertility and sexual health as part of cancer treatment.
Action Steps:
- Increase insurance coverage and reimbursement for sexual health and fertility planning services and discussions before, during, and after treatment for certain cancers.
- Develop protocols for protecting the fertility options of cancer patients prior to treatment and include survivors in decision making about fertility.
- Address sexual intimacy and other quality of life (e.g., fertility, gender reassignment surgery) concerns as they relate to treatment options (source).
Strategy D: Reduce cancer care costs incurred by patients and families.
Action Steps:
- Educate policymakers on the impact of financial stress on cancer care outcomes.
- Educate patients about substandard insurance coverage, and monitoring for the expansion of those and/or thinking about limiting some of those products (for example, short-term limited duration plans and healthcare sharing ministries).
- Encourage financial navigators to inform patients before a surgery/admission/procedure to let them know upfront costs and minimize surprise medical bills (source).
- Reduce out of pocket costs supporting cancer treatment and associated expenses.
- Increase patient access to copay and financial counseling assistance.
Priority 4: Empower patients and providers to communicate about advance care planning early in the cancer treatment journey.
Strategy A: Increase awareness of the importance of advance care planning.
Action Steps:
- Increase public awareness about the importance of advance care planning conversations (source).
- Provide patient and family education on the importance of advanced care planning.
- Provide culturally and linguistically appropriate resources on advanced care planning for providers, cancer patients, and their families (source).
- Provide patient and family education on the importance of advanced directives and how to ask for them (source).
- Develop best practice clinic workflow models to ensure advance care planning conversations are part of adult primary care and part of regularly reviewed patient health history (source).
- Educate providers on the need for and the reimbursement of advanced directives conversations (source).
Strategy B: Improve accessibility of advance care planning documents across health systems.
Action Steps:
- Ensure that advance care planning documents are consistently and reliably stored in electronic health records and accessible within and across medical settings (source).
- Promote access to and utilization of quality state-approved advanced care documents.
- Support efforts to improve electronic health records and patient charts to include easy access to advance care planning documents for providers and patients (source).
- Provide the patient and family multiple opportunities and tools for initiating conversations related to advance care planning (source).
- Employ community health workers to encourage and assist patients in completing advance care planning documents (source).
Strategy C: Create health system strategies to routinely assess and review advance care plans throughout the cancer experience, including diagnosis, treatment, survivorship, and end of life.
Action Steps:
- Integrate advance care planning into survivorship services at the beginning of treatment (source).
- Develop models or algorithms for reviewing patient advance care plans throughout the cancer experience (source).
- Develop uniform system-wide methods for making quality advanced care documents readily available (source).
- Collect data and quality measures at the health care system level about the number of advance care planning conversations and patient/family satisfaction with conversations (source).
Priority 5: Increase patient and caregiver access to non-clinical support services.
Strategy A: Increase insurance coverage for non-clinical support services for survivors and caregivers.
Action Steps:
- Educate health insurance companies on the needs for and benefits of non-clinical support services (source).
- Increase insurance coverage and availability of financial navigators, patient navigators, and other support services (source).
- Educate policymakers on the needs for and benefits of non-clinical support services.
- Educate employers on the needs for and benefits of non-clinical support services.
Strategy B: Increase the availability of non-clinical support services for patients and caregivers including financial counseling and assistance, patient education, and patient navigation.
Action Steps:
- Adopt distress/symptom assessment tools and workflow models that identify the physical, social, psychological, and spiritual needs of patients early within their cancer treatment (source).
- Develop systems that make support and care coordination services available to all cancer patients and survivors (source).
- Educate health care providers on how to assess physical, psychological, social, and spiritual distress in their patients (source).
- Utilize patient navigators to help patients and caregivers access support services and care coordination (source).
- Work with communities to develop and implement culturally and linguistically appropriate resources for patients and families (source).
- Identify and address gaps in access to non-clinical support services for underserved populations (source).
- Incorporate evidence-based complementary and alternative therapies into survivorship care programs.
- Establish a plan to provide equitable access to non-clinical support services for survivors and caregivers during public health emergencies (source).
- Educate human resource professionals as to the full extent of resources available to childhood cancer caregivers through the Family Medical Leave Act (FMLA) (source).
- Educate patients, parents, K-12 educators, and school counselors on the physical, emotional, and cognitive impacts of childhood cancer and on the supports available through the school systems (Individualized Education Plan [IEP], educational consultants, etc.) (source).
- Reduce structural barriers to healthcare access by supporting patient navigation programs and the employment of social workers to provide childhood cancer care (source).
- Use community health workers, patient navigators, churches, and community support programs, especially in underserved communities, to assist with reducing structural barriers. This includes assisting with scheduling appointments, providing transportation, providing language translation, and providing childcare (source).
- Increase support for state or regional transportation assistance programs, including transportation options for cancer patients (children and adults) and their families who live in rural and underserved areas (source).
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Priority 6: Enhance awareness of and participation in cancer research of all types, and accelerate scientific findings into policy and practice.
Strategy A: Develop public awareness campaigns to build support for cancer-related research.
Action Steps:
- Support all types of cancer research, including basic, translational, clinical, and population research.
- Align cancer research initiatives to promote equity in care, elevate the voice and power of the community in research, address bias, and build empathy in care.
- Develop and implement culturally appropriate education and outreach campaigns about cancer research to inform and build trust with patients and communities.
- Develop and implement public education campaigns to promote cancer clinical trials.
- Work with communities to develop culturally and linguistically appropriate tools and resources to increase knowledge and participation in cancer research.
- Educate policymakers on the benefits of funding cancer research and clinical trials.
- Increase funding for cancer research of all types.
- Support policies and systems changes that expand access to and use of clinical trials.
- Facilitate collaboration and communication in cancer research.
- Reduce barriers to developing, accessing, and translating research.
- Increase collaboration between researchers and communities to translate research findings into practice.
- Develop and implement education and outreach campaigns to inform health care providers and clinical staff about the benefits of offering clinical trials.
- Engage cancer survivors as peer educators to increase participation in cancer clinical trials.
- Build and sustain coalitions with key stakeholders to enhance support for cancer research and the availability of cancer clinical trials.
- Highlight cancer research collaborations between local and regional cancer centers.
- Identify and address the need for consumer-friendly explanations of childhood cancer clinical trials, informed consent, and referral patterns (source).
- Encourage hospitals to identify and enroll in national research/clinical trials such as Children’s Oncology Group research, NCI research, and LLS’s Dare to Dream Project, as well as clinical trial navigation from LLS’s Clinical Trial Support Center (source).
Strategy B: Support efforts to increase access and comprehensive coverage for cancer research and clinical trials.
Action Steps:
- Ensure every oncology patient in Iowa is offered, understands, and has equitable access to cancer-related clinical trials.
- Decrease barriers to participating in cancer-related clinical trials, including geographic location, insurance status, transportation, loss of wages or other job concerns, and lack of culturally -affirming resources.
- Increase the number and location of community oncology practice clinical research sites.
- Link the clinical research efforts of Iowa’s NCI-designated Holden Comprehensive Cancer Center at the University of Iowa with collaborating practices throughout the state for enhanced access to emerging treatment and interventions.
- Fund, develop, and manage systems and tools to help people in Iowa find complete information about open clinical trials.
- Develop resources for patients and providers on cancer clinical trials and health insurance.
- Promote training opportunities for health care providers on the importance and availability of cancer clinical trials.
- Increase public and private insurance coverage of medical and non-medical expenses incurred by participating in cancer clinical trials.
- Monitor state and federal legislation regarding funding for cancer research and clinical trials.
- Work with state and national partners to support funding for childhood cancer research (source).
Strategy C: Provide patient navigation and support throughout the clinical trials process.
Action Steps:
- Develop and implement provider reminder systems to identify potential patients eligible for clinical trials.
- Build relationships and improve communication between oncology practices to streamline referral of patients to sites where clinical trials are most easily accessible to them.
- Employ community health workers to support patients’ comprehensive understanding and informed decision-making in regards to cancer clinical trials.
- Develop and test clinical trial consent forms using principles of health literacy.
- Establish language initiatives to help cancer clinical trial investigators enhance recruitment and management of patients with limited English proficiency.
- Identify and promote evidence-based strategies and best-practices to increase utilization and accrual of patients into clinical trials.
- Utilize technology and community resources to reduce transportation barriers to accessing cancer clinical trials for all Iowans, including those who reside in rural areas.
- Establish a plan to provide equitable access to cancer clinical trials during public health emergencies.
- Discuss ways for patients to participate in research, in addition to clinical trials.
Strategy D: Increase recruitment and inclusion of populations traditionally underrepresented in cancer research and clinical trials.
Action Steps:
- Develop and track statewide measures of clinical trials recruitment, enrollment, retention, and equity.
- Identify and address barriers to clinical trial participation such as fear, cultural beliefs, and potential medical and non-medical expenses.
- Work alongside communities to develop culturally and linguistically appropriate tools and resources to increase trust and acceptance of cancer research.
- Establish benchmarks for the recruitment of each underrepresented population.
- Ensure the inclusion of LGBTQ+ individuals in all private and public human subjects cancer research.
- Identify and respond to gaps in cancer-related data through research.
- Invest and support a diverse cancer research workforce.
Strategy E: Expand research infrastructure for all types of clinical and observational studies, developing and streamlining methods to increase access to participation for all.
Action Steps:
- Enable every patient to contribute their health data and biospecimens to research in a secure, privacy-protected manner that honors their wishes for the use of these resources to conduct cancer research.
- Facilitate rapid referral, access, enrollment, accrual, and retention of diverse populations in clinical trials.
- Conduct research to identify and overcome barriers to the treatment of early-stage cancers in communities with disparities, including financial toxicity and policies that limit effective system-level and community-sourced patient navigation services.
- Integrate clinical research into routine clinical care using methods that avoid increasing provider or patient burden.
- Ensure that opportunities to participate in and benefit from research are equitably distributed.
- Develop and implement methods to return research results in meaningful ways to patients who participate in studies.
Data Targets
Priority 7: Ensure early access to palliative care.
Strategy A: Educate the public about palliative care.
Action Steps:
- Create a public awareness campaign to inform the public on the benefits of palliative care, emphasizing its importance beyond end-of-life care (source).
- Educate providers, patients, and caregivers that palliative care is also available for symptom relief during treatment, not just at end-of-life (source).
- Provide targeted, culturally and linguistically appropriate palliative care educational information to patients and caregivers (source).
- Improve the assessment and treatment of pain and other symptom management by including pain assessments at each follow-up visit (source).
- Educate health care providers on how to assess physical, psychological, social, and spiritual distress in their patients (source).
- Educate the entire clinic team on palliative care and its benefits in cancer care.
- Work with communities and community health workers to provide culturally and linguistically appropriate palliative care information to the public, patients, and families (source).
- Educate patients with non-curative cancer about palliative care and its role early in their treatment (source).
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Strategy B: Increase provider use of palliative care guidelines and quality standards.
Action Steps:
- Train health care providers and support service professionals on how to conduct culturally and linguistically appropriate palliative care conversations between cancer patients and their families (source).
- Follow clinical guidelines and create systems/workflows to identify patients who could benefit from palliative care consultation (source).
- Create electronic health record algorithms for the delivery of palliative care standards (source).
- Develop statewide publicly reported metrics for provider adherence to palliative care standards (source).
- Develop provider incentives for compliance with the American Society of Clinical Oncology (ASCO), American Academy of Hospice and Palliative Medicine (AAHPM), and National Comprehensive Cancer Network (NCCN) standards (source).
- Collect data on the use of palliative care during treatment and compliance with standards (source).
Strategy C: Reduce barriers to quality palliative care.
Action Steps:
- Develop culturally and linguistically appropriate tools that make it simpler for patients and families to request palliative care consultations (source).
- Inform providers, patients, and caregivers that palliative care is also available for symptom relief during treatment, not just end of life (source).
- Provide patients and families multiple opportunities and tools for initiating conversations related to palliative care throughout treatment (source).
- Advocate for insurance coverage of palliative care consultations and services.
- Focus on outpatient, home-based and community clinic-based palliative care in rural communities.
- Promote increased access to integrated palliative care services for children facing any stage of cancer (source).
Data Targets
Priority 8: Provide high-quality childhood cancer care.
Strategy A: Educate Iowans about childhood cancer and methods to support patients/families.
Action Steps:
- Provide educational opportunities for community members focused on childhood cancer (including Iowa cancer incidence/mortality data, research, and ways to best support patients and their families.
- Offer free or low-cost educational sessions for school administrators, teachers, support staff, and students on how to best support a child during and after their cancer treatment (i.e. educational consultants, establish an individualized education plan [IEP]).
- Support organizations working to reduce the burden of childhood cancer in Iowa.
- Educate Iowans on the early signs of childhood cancer.
- Advocate for children in Iowa to have access to quality health insurance coverage.
Strategy B: Provide continued training for health providers about childhood cancer.
Action Steps:
- Whenever possible, advocate for in-person childhood physical examinations to reduce the chances of missing markers or signs of childhood cancer due to incomprehensiveness associated with telehealth visits.
- Promote the early diagnosis and timely referral/access to a childhood cancer center.
- Train providers to recognize and support the unique needs of childhood cancer patients throughout their lifespan, including coping with the late-effects of treatment, fertility preservation, mental health, education, and financial barriers.
- Conduct a needs assessment for subpopulations, groups, or locations disproportionately impacted by childhood cancer for evidenced-based resources, with special attention to marginalized, BIPOC, and/or LGBTQ+ communities.
- Encourage parents/caregivers to keep the child up-to-date on their routine immunizations like the flu shot to prevent unnecessary illness or infection, while also informing them about vaccination changes while the child is undergoing treatment (no live vaccines such as MMR, Varicella, Oral Polio).
- Promote use of recommendations/standards for follow-up care (e.g. COG Passport for Care; Psychosocial Standards of Care Project for Childhood Cancer), including baselines for neuro-cognitive status and follow-up screening (source).
Strategy C: Enhance access to quality support services for childhood cancer patients and their families, especially around mental health.
Action Steps:
- Increase access to support programs/resources to assist the whole family (i.e. patient, parents, and siblings) throughout the childhood cancer journey, including psychosocial and emotional support services.
- Improve local access to mental health resources and support groups for children and families with cancer.
- Incorporate evidence-based complementary and alternative therapies (CAM) into childhood cancer care programs.
- Create opportunities for childhood /AYA survivorship coordinators and navigators located in childhood and adult oncology centers to share best-practices.
- Improve access to programs to support family/caregiver needs (diagnosis, treatment, late effects, psychosocial support programs, sibling support, respite care).
- Ensure access to childhood palliative/hospice care programs.
- Create a toolkit or website with all available resources for survivors and their families on what to do after recovery to live a long, happy life including long-term follow-up care.
- Ensure that treatment locations provide childhood cancer patients and their families with a list of local resources and an annual reminder and patient assessment (source).
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Strategy D: Reduce the financial burden of childhood cancer.
Action Steps:
- Examine currently available programs and resources supporting emerging drugs, therapies, and clinical trials.
- Ensure all children have health insurance.
- Improve access to financial assistance programs with engaged financial navigators/advisors.
- Expand transportation and lodging assistance programs for children with cancer and their families while they complete cancer treatment.
- Educate elected officials on the unique needs and disparities experienced by patients and families facing a childhood cancer diagnosis (i.e. associated childcare costs for siblings of cancer patients; work-related assistance for parents/caregivers; travel costs, and funding to support biomarker testing and clinical trials).
Strategy E: Recognize the need for enhanced research support for childhood cancers, including improved mechanisms for pediatric drug development.
Action Steps:
- Support the use of basic/molecular research to better understand the causes of childhood cancers.
- Develop consumer-friendly explanations of clinical trials, informed consent, and referral patterns.
- Increase access to genetic testing and biomarker profiling.
- Make all phases of clinical trials more available to patients.
- Support funding for childhood cancer research leading to new therapies targeted specifically for children with cancer that are effective and less toxic (ACCO).
- Promote research to improve the quality of life for survivors that address the physical, cognitive, and psychosocial consequences of treatment from diagnosis through late effects.
- Increase access to all phases of childhood oncology clinical trials (source).
References:
- Above + Beyond Cancer AYA Program: https://aboveandbeyondcancer.org/young-adult-survivor-program
- American Cancer Society: https://www.cancer.org/cancer/cancer-in-children/types-of-childhood-cancers.html
- American Childhood Cancer Organization: https://www.acco.org/
- Children’s Cancer Connection: https://childrenscancerconnection.org/
- Children’s Oncology Group (COG) Supportive Care Endorsed Guidelines: https://childrensoncologygroup.org/cog-supportive-care-guidelines
- National Cancer Institute: https://www.cancer.gov/types/childhood-cancers
- St. Baldrick’s Foundation and Family Handbook: https://www.childrensoncologygroup.org/downloads/English_COG_Family_Handbook.pdf
- Triage Cancer: https://triagecancer.org/
Priority 9: Provide high-quality adolescent and young adult (AYA) oncology care.
Strategy A: Educate Iowans about AYA cancers and methods to support patients/families.
Action Steps:
- Provide educational opportunities for community members focused on AYA cancers (including Iowa cancer incidence/mortality data, research, and ways to best support patients and their families.
- Offer free or low-cost educational sessions for school administrators, teachers, support staff, and students on how to best support an adolescent/young adult during and after their cancer treatment (i.e. educational consultants, establish an individualized education plan [IEP]).
- Support organizations working to reduce the burden of AYA cancers in Iowa.
- Educate Iowans on the early signs of cancer, especially for those under age 39.
- Ensure patients have access to affordable/quality health insurance coverage both before and during treatment.
Strategy B: Provide continued training for health providers about AYA cancers.
Action Steps:
- Whenever possible, advocate for in-person childhood and young adult physical examinations to reduce the chances of missing markers or signs of AYA cancers due to incomprehensiveness associated with telehealth visits.
- Encourage providers to refer patients to cancer centers affiliated with the Children’s Oncology Group (COG), NCI-Designated Cancer Center, and/or a clinical research network such as NCTN or NCORP.
- Train providers to recognize and support the unique needs of AYA cancer patients throughout their lifespan, including coping with the late-effects of treatment, fertility preservation, mental health, education, career planning and financial barriers.
- Conduct a needs assessment for subpopulations, groups, or locations disproportionately impacted by AYA cancers for evidenced-based resources, with special attention to marginalized, BIPOC, and/or LGBTQ+ communities.
- Encourage patients to stay up-to-date on their routine immunizations like the flu shot to prevent unnecessary illness or infection, while also informing them about vaccination changes while undergoing treatment (no live vaccines such as MMR, Varicella, Oral Polio).
Strategy C: Enhance access to quality support services for childhood/AYA cancer patients and their families, especially around mental health and social support.
Action Steps:
- Increase access to support programs/resources to assist the whole family (i.e. patient, parents, and siblings) throughout the AYA cancer journey, including psychosocial and emotional support services.
- Improve local access to mental health resources and support groups for adolescents/young adults and families with cancer.
- Incorporate evidence-based complementary and alternative therapies (CAM) into survivorship care programs.
- Create opportunities for childhood/AYA survivorship coordinators and navigators located in childhood and adult oncology centers to share best-practices.
- Consider online outreach and support to provide peer social support to AYAs with cancer (source).
- Improve access to programs to support family/caregiver needs (diagnosis, treatment, late effects, psychosocial support programs, sibling support, respite care).
- Ensure access to AYA-focused palliative/hospice care programs.
- Create a toolkit or website with all available resources for survivors and their families on what to do after recovery to live a long, happy life with long-term follow-up care.
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Strategy D: Reduce the financial burdens associated with AYA cancers.
Action Steps:
- Examine currently available programs and resources supporting emerging drugs, therapies, and clinical trials.
- Ensure all adolescents and young adults have health insurance.
- Improve access to financial assistance programs with engaged financial navigators/advisors.
- Expand transportation and lodging assistance programs for adolescents and young adults with cancer and their families while they complete cancer treatment.
- Educate elected officials on the unique needs and disparities experienced by patients and families facing an AYA cancer diagnosis (i.e. associated childcare costs for siblings of cancer patients; work-related assistance for parents/caregivers; travel costs, and funding to support biomarker testing and clinical trials).
Strategy E: Expand options for the reproductive future of cancer survivors.
Action Steps:
- Encourage providers to use evidence-based tools to assist health care providers navigate fertility preservation options discussions with their patients (source).
- Discuss fertility preservation with all patients of reproductive age (and with parents or guardians of children and adolescents) if interfertility is a potential risk of therapy) (source).
- Refer patients who express an interest in fertility preservation (and patients who are ambivalent) to reproductive specialists (source).
- Address fertility preservation as early as possible, before treatment starts (source).
- Document fertility preservation discussions in the medical record (source).
- Answer basic questions about whether fertility preservation may have an impact on successful cancer treatment (source).
- Refer patients to psychosocial providers if they experience distress about potential infertility (source).
- Encourage patients to participate in registries and clinical studies (source).
Strategy D: Recognize the need for enhanced research support for AYA cancers.
Action Steps:
- Support the use of basic/molecular research to better understand the causes of AYA cancers.
- Develop consumer-friendly explanations of clinical trials, informed consent, and referral patterns.
- Increase access to genetic testing and biomarker profiling.
- Make all phases of clinical trials more available to patients.
- Support funding for childhood/AYA cancer research leading to new therapies targeted specifically for adolescents and young adults with cancer that are effective and less toxic (ACCO).
- Promote research to improve the quality of life for survivors that address the physical, cognitive, and psychosocial consequences of treatment from diagnosis through late effects.
References:
- American Childhood Cancer Organization: https://www.acco.org/
- Children’s Oncology Group (COG) Supportive Care Endorsed Guidelines https://childrensoncologygroup.org/cog-supportive-care-guidelines
- FORCE: https://www.facingourrisk.org/
- National Cancer Institute: https://www.cancer.gov/types/aya
- Imerman Angels: https://imermanangels.org/
- Livestrong Fertility: https://www.livestrong.org/what-we-do/program/fertility
- Stupid Cancer: https://stupidcancer.org/
- Ulman Foundation: https://ulmanfoundation.org/
- Young Survival Coalition: https://www.youngsurvival.org/
Priority 10: Ensure patients undergoing treatment are prepared for a natural disaster and/or emergency.
Action Steps:
- Educate patients what to do ‘in case of emergency’ in the event of a natural disaster or emergency (i.e. flooding, tornado, derecho, pandemic). Examples of information to include here and here.
- Provide patients with a wallet card with space for critical treatment information that they can bring to a provider during a disaster. Example: National Cancer Institute and the American Society of Clinical Oncology (ASCO) created a cancer treatment during a disaster wallet card (available in English and Spanish).
References:
- Centers for Disease Control and Prevention. https://www.cdc.gov/cancer-survivors/patients/be-prepared-for-an-emergency.html
Chapter 5
Survivorship and End-of-Life Care
Chapter 5 Overview
Select a priority to learn more
- Priority 1 Utilize best-practices to support a cancer patient’s transition from active treatment to post-treatment care.
- Priority 2 Increase provider, patient, and caregiver awareness of the importance of cancer risk reduction behaviors and cancer screening for cancer survivors.
- Priority 3 Achieve excellent quality of life for all Iowans with cancer and their caregivers.
- Priority 4 Improve long-term follow-up care for childhood cancer survivors.
- Priority 5 Increase availability and access to quality end-of-life care.
Ensure resources to optimize quality of life for cancer survivors and their families.
The American Cancer Society uses the term “cancer survivor” to refer to anyone who has ever been diagnosed with cancer no matter where they are in the course of their disease.
Continued scientific advances in screening and treatment have allowed those diagnosed with cancer to live longer than ever before. According to the Iowa Cancer Registry, Iowa has estimated 159,700 cancer survivors among Iowans (source). As Iowa’s population continues to grow and age, so will the number of cancer diagnoses, patients and survivors.
Iowans face unique challenges following a cancer diagnosis, as cancer treatments can cause a variety of short- and long-term effects impacting the patient and their family. Survivorship experiences differ based on a person’s unique experience and may include:
- Late and long-term effects of treatment, especially pediatric and adolescent cancer treatments.
- Treating cancer as a chronic illness (if cancer doesn’t go away).
- Fears of cancer recurrence (if cancer comes back).
- Screening/Early-Detection for second cancers (if someone has another type of cancer).
- Seeking support for mental health including treatment for post-traumatic stress disorder.
- Addressing fertility, fertility assistance, and pregnancy after cancer.
- Managing health care after cancer, including follow-up care and wellness support services.
- Access to palliative care, supportive care, and hospice at the right time.
- Support for family members, friends and caregivers as part of the survivorship experience.
It is important to remember the unique survivorship needs for people diagnosed with childhood cancer, as they differ from the needs of adults with cancer. Support includes not only the patient but also parents, siblings, family members and often their community support system. Survivors of childhood cancer require lifelong surveillance because late effects contribute to significant morbidity among adults who were treated for cancer during childhood, approximately 60-90% of patients with childhood cancer develop one or more chronic health conditions, and 20-80% experience severe or life-threatening complications during adulthood.
Stories from the Iowa Cancer Plan
Data Targets
Priority 1: Utilize best-practices to support a cancer patient’s transition from active treatment to post-treatment care.
Strategy A: Educate policymakers and the public about key issues in cancer survivorship.
Action Steps:
- Health care providers, patient advocates, and other stakeholders should work to raise awareness of the needs of cancer survivors, establish cancer survivorship as a distinct phase of cancer care, and act to ensure the delivery of appropriate survivorship care (NAM, 2006).
- Encourage insurers and payers of health care to recognize survivorship care as an essential part of cancer care and design benefits, payment policies, and reimbursement mechanisms to facilitate coverage for evidence-based aspects of care (NAM, 2006).
- Improve the quality of life of cancer survivors through policies to ensure their access to psychosocial services, fair employment practices, and health insurance (NAM, 2006).
- Empower oncology providers, advocacy organizations, and patients to educate employers and the public about the successes achieved in cancer treatment, the improved prospects for survival, and the continuing productivity of most patients who are treated for cancer (NAM, 2006).
- Create educational events or policy briefs directed at policymakers to inform them on key issues in cancer care and survivorship.
- Identify and address health inequities in survivor populations (source).
- Employers should implement programs to assist cancer survivors, for example, through short- and long-term disability insurance, return-to-work programs, accommodation of special needs, and employee assistance programs (NAM, 2006).
- Work with public health economists to calculate the financial impacts of childhood cancer in the state such as loss of income by parents, out-of-pocket costs for care, data on financial hardships/medical bankruptcy, and long-term financial impacts on childhood cancer survivors such as employability and insurability (source).
Strategy B: Streamline clinical transitions for patients moving from active to post-treatment care.
Action Steps:
- Encourage health care providers to use evidence-based clinical practice guidelines, assessment tools, and screening instruments to help identify and manage late effects of cancer and its treatment (NAM, 2006).
- Educate insurance companies about the benefits of paying for the integration of cancer survivor services and the transition to primary care treatment (source).
- Assemble community-based resource guides for survivors and health care providers (NAM, 2006).
- Expand educational opportunities for health care providers to equip them to address the unique health care and quality of life issues facing cancer survivors on topics such as sexual health, physical activity, nutrition, fertility, depression and anxiety (NAM, 2006).
- Encourage health care systems to invest in the integration of cancer survivor services and the transition to primary care (source).
- Provide robust post-treatment survivorship care, including a survivorship care plan with a treatment summary and personalized recommendations for monitoring and follow-up care (source).
- Provide individualized survivor care plans to survivors with information specific to their treatment and ongoing health needs (source).
- Provide individualized survivor care plans to the survivor’s primary care team with information specific to the survivor’s treatment and ongoing health needs (source).
Strategy C: Increase linkages to community support services for cancer survivors.
Action Steps:
- Employ patient navigators and community health workers to help patients and caregivers access survivorship services.
- Increase the availability and use of cancer rehabilitation and wellness services in communities and virtually.
- Create community- or region-wide partnerships to leverage and share survivorship resources across organizations (source).
- Work with communities to develop and/or promote culturally and linguistically appropriate survivorship support services.
- Offer LGBTQ+ cancer survivors access to culturally competent support services either through the creation of LGBTQ+ -specific support groups, referrals to community groups, or at a minimum training support service staff to provide LGBTQ+ culturally competent care (source).
- Assess gaps in access and use of non-clinical support services for underserved populations (source).
- Establish a plan to provide equitable access to community support services for survivors and caregivers during public health emergencies (source).
- Work with stakeholders to create and maintain a comprehensive list of childhood cancer resources for childhood cancer patients and their families, to be distributed at all treatment locations (source).
- Support programs that teach self-advocacy to survivors of childhood cancer before they transition to an adult health system (source).
Strategy D: Support research focused on cancer survivorship.
Action Steps:
- Include patient and cancer survivor representation and input in research projects.
Priority 2: Increase provider, patient, and caregiver awareness of the importance of cancer risk reduction behaviors and cancer screening for cancer survivors.
Strategy A: Tailor cancer risk reduction messages and activities to meet the unique needs of cancer survivors.
Action Steps:
- Educate survivors on the importance of regular check-ups with their primary care provider for overall health (source).
- Provide access to primary and secondary prevention services (e.g., smoking cessation, cancer screening) (NAM, 2006).
- Educate survivors and caregivers on maintaining a healthy lifestyle as a way to decrease the risk of cancer recurrence and side effects from treatment (source).
- Encourage survivors to regularly participate in physical activity in safe and empowering ways (source).
- Support workplace policies to prevent and reduce excessive drinking and programs that emphasize the importance of healthy eating during and after cancer treatment (source).
- Gather and incorporate the survivor perspective into risk reduction messaging and activities.
- Educate primary care teams on the increased importance of risk reduction behaviors (source).
- Include the long-term risks of treatment (including second cancers) in discussions before, during, and after treatment for certain cancers.
- Support partners in developing specific patient navigation programs addressing the needs of disparate populations including AYA survivors, rural populations, racial/ethnic minorities, LGBTQ+, individuals, etc.
Strategy B: Tailor cancer early-detection and screening messages to meet the unique needs of cancer survivors.
Action Steps:
- Educate survivors about their potential risk for secondary cancers due to treatment exposures (source).
- Integrate risk assessment tools within primary care teams to provide tailored evidence-based screening recommendations to cancer survivors (source).
- Educate survivors on when and how to get screened for cancers, and include in individualized survivor care plans to survivors with information specific to their treatment and ongoing health.
- Implement a tailored approach to increase the utilization of recommended cancer screenings among cancer survivors (source).
- Educate communities about risk factors that may change standard cancer screening recommendations (source).
- Forecast screening activities in patient-accessed electronic health records (source).
Resources:
Priority 3: Achieve excellent quality of life for all Iowans with cancer and their caregivers.
Strategy A: Provide non-clinical services to cancer survivors to support their quality of life.
Action Steps:
- Increase patient and caregiver access to psychosocial, wellness, financial, sexual, spiritual, rehabilitation and community-based support services.
- Implement collaborative care models for the management of distress and/or psychiatric disorders (source).
- Helping cancer survivors who live in rural areas cope with cancer-related anxiety and distress with “telehealth” approaches such as therapy and other psychosocial support delivered by phone, mobile apps, and websites.
- Support programs that facilitate job training for childhood cancer survivors (source).
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Data Targets
Priority 4: Improve long-term follow-up care for childhood cancer survivors.
Strategy A: Educate the public and health providers about the long-term effects of childhood cancer treatment and the unique needs of survivors.
Action Steps:
- Cancer providers, advocacy organizations, NCI, and other government agencies should continue to educate employers and the public about the successes achieved in cancer treatment, the improved prospects for survival, and the continuing productivity of most patients who are treated for cancer (NAM, 2006).
- Increase access, awareness and use of physical, psychosocial and financial support services.
- Offer educational opportunities for school administrators, teachers, support staff, and students on how to support a child during and after cancer treatment.
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Strategy B: Support follow-up care for childhood cancer survivors.
Action Steps:
- Provide cultural and age appropriate cancer services to LGBT youth survivors (source).
- Establish health systems-level quality improvement metrics and processes to improve transitions from active treatment to post-treatment care.
- Increase the number of health professionals trained in adult and pediatric palliative care.
Strategy C: Increase access to programs supporting childhood cancer survivors and their families.
Action Steps:
- Insurers and payers of health care should recognize survivorship care as an essential part of cancer care and design benefits, payment policies, and reimbursement mechanisms to facilitate coverage for evidence-based aspects of care (NAM, 2006).
- Ensure all cancer survivors have access to adequate and affordable health insurance.
- Increase utilization and effectiveness of survivorship care programs.
- Increase community-clinical linkages to community support services (source).
- Educate health care providers on the importance of early and regular conversations with patients on goals of care, including patients’ cultural preferences.
- Educate health care providers, patients, families and communities on the specific and unique needs of cancer survivors, including sexual health, physical activity, nutrition, fertility, depression and anxiety.
- Promote areawide community-based resource guides for survivors and health care providers (NAM, 2006).
- Increase resources and support for the unique needs of caregivers.
Strategy D: Enhance research on quality of life issues.
Action Steps:
- TBD
Priority 5: Increase availability and access to quality end-of-life care.
Strategy A: Increase awareness of the benefits of palliative care at the end of life.
Action Steps:
- Create a public awareness campaign to inform the public about the benefits of palliative care and hospice care, and the differences between them.
- Educate health care providers, patients, caregivers and the community on the benefits of starting palliative care at the time of a cancer diagnosis.
- Work with community organizations and community health workers to provide culturally and linguistically appropriate information on palliative care to the public (source).
Strategy B: Reduce barriers to access quality palliative care.
Action Steps:
- Educate health care providers on how to assess physical, psychological, social, and spiritual distress in their patients (source).
- Increase access to evidence-based interventions for cancer pain management, palliative care, and wellness (source).
- Educate providers, patients, and caregivers that palliative care can occur in or out of hospice settings (source).
- Increase the number of qualified palliative care providers (source).
- Promote additional training and certification for other providers and allied staff (nurses, LPNs, CNAs, etc.) in palliative care (source).
- Increase insurance coverage of palliative care conversations and services (source).
- Increase access to palliative care services for all cancer patients and increase access to hospice services for patients facing end of life.
- Create electronic health record algorithms for the delivery of palliative care standards (source).
- Develop culturally and linguistically appropriate tools that make it simpler for patients and families to request palliative care consultations (source).
- Incorporate the cancer perspective while addressing widespread opioid abuse issues.
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support, the Lifeline network is available 24/7 across the United States.
Strategy C: Increase cancer patient referrals to and utilization of hospice services.
Action Steps:
- Provide culturally and linguistically appropriate resources on end-of-life care for providers, cancer patients, and their families (source).
- Promote and provide culturally and linguistically appropriate bereavement services to patients and families (source).
- Educate health care teams on the importance of respecting and supporting decisions of the cancer patient and their family (source).
- Create and distribute a hospice toolkit that includes resources, forms, and regulations for hospice services (source).
- Promote the establishment of a health care power of attorney, living will, and end-of-life wishes early in diagnosis, so that the patient’s wishes will be known (source).
- Establish a plan to provide equitable access to quality end-of-life care during public health emergencies (source).
- Advertise continuing education opportunities for health care providers in pain management or palliative care (source).
- Educate health care professionals about tools and resources they can use to facilitate meaningful, culturally relevant conversations with patients and families about palliative and end-of-life care (source).
- Develop provider incentives for compliance with the American Society of Clinical Oncology (ASCO), American Academy of Hospice and Palliative Medicine (AAHPM), and National Comprehensive Cancer Network (NCCN) standards (source).
- Develop statewide publicly reported metrics for provider adherence to palliative care standards (source).
- Support policies, systems change, research, and programs that increase the availability of culturally competent end-of-life and palliative care for the LGBTQ+ community (source).
- Support training for palliative care and hospice providers on LGBTQ+ cultural competence (source).
- At the end-of-life, dignified death is a priority for LGBTQ+ patients. Unique topics such as continuation of hormone therapy for transgender patients as well as respect for patient choice of burial and death rituals need to be addressed (source).
- Provide ongoing training to all hospice/palliative care providers and staff to ensure culturally competent care to LGBTQ+ patients and families of choice in all care settings (including hospice, long-term care, and skilled nursing facilities) (source).
- Address the complex spiritual needs of LGBTQ+ patients and families of choice with awareness of the fear and distrust of faith-based communities experienced by many LGBTQ+ communities. This includes respecting the choice of not wanting spiritual/pastoral care (source).
- Advance palliative care in national quality measurement and performance improvement strategies to ensure a focus on high-value patient- and family-centered outcomes across the continuum of care, including promoting the development and use of meaningful metrics and benchmarks for quality reporting and value-based reimbursement (source).
- Ensure comprehensive, timely access to and effective management of prescription medications for patients with medically appropriate, evidence-based indications while recognizing the public health imperative to curb prescription drug misuse and diversion and collaborating with professional, regulatory and industry stakeholders to maximize individual and public safety and minimize undue prescriber burden (source).
- Provide in-person and/ or virtual access to culturally competent and/or LGBTQ+-specific bereavement programs for LGBTQ+ support networks (i.e., family of choice), recognizing the increased risk for disenfranchised grief (source).
Strategy D: Support research and best-practice sharing for end-of-life care.
Action Steps:
- Create a report card by county or region to measure the percentage of cancer patient referrals and length of stay in hospice (source).
- Increase state-level surveillance of cancer survivors.
- Identify and address health inequities in cancer survivorship among Iowa’s populations.
- Fund and conduct research projects to measure the effectiveness of non-clinical approaches on cancer survivor quality of life.
- Increase funding for palliative care and hospice research, particularly research focused on historically marginalized groups, to strengthen clinical practice and improve healthcare delivery and outcomes for all patients living with multiple chronic conditions or life-threatening or serious illness, as well as their families and caregivers (source, source).
- Conduct research on the end-of-life/chronic illness experiences of LGBTQ+ patients and their caregivers, including the development of LGBTQ+-specific psychosocial, spirituality, and existential distress measures (source).
Resources:
- Get Palliative Care: https://getpalliativecare.org/
- CaringInfo: https://www.caringinfo.org/
- https://www.capc.org/
- American Cancer Society’s Cancer Helpline: 1-800-227-2345 or virtual chat https://www.cancer.org/about-us/online-help/contact-us.html