Cancer Screening & Early Detection Toolkit
Introduction
Cancer screening tests find cancer in the body before a person has any symptoms. Screening for cancer does not necessarily mean a person has or will develop cancer. It can help find cancer early if done routinely, which makes it easier to treat or cure before it has spread to other parts of the body. Different cancer screening tests include physical exams, laboratory tests, imaging procedures, genetic tests, and patient histories (source).
There are many barriers to cancer screening access, including time, transportation, and cost (source). Other common barriers are lack of awareness and fear, which the Iowa Cancer Consortium’s Cancer Screening & Early Detection Workgroup aims to address through this toolkit. The information below on cancer screenings and recommended guidelines is not meant to replace conversations with medical providers, but rather enhance them and help close information gaps before even stepping into a medical facility.
Recommendations for cancer screenings depend on your age, family history, and other risk factors. The most common source for these guidelines is the U.S. Preventive Services Task Force (USPSTF). Other organizations like the American Cancer Society, National Comprehensive Cancer Network (NCCN), and specialized medical associations provide their own guidelines. We will be referring to USPSTF recommended guidelines throughout this toolkit, since they determine what procedures insurers will cover. Insurers must cover services that have an “A” or “B” rating from USPSTF, meaning that “there is a high certainty that the services have a substantial or moderate net health benefit.” (source)
Some cancers do not have recommended routine screening guidelines from USPSTF. This could be due to insufficient evidence of the health benefits of these screenings or concern about overdiagnosis. However, additional cancer screenings for oropharyngeal (head and neck), prostate, anal, and skin cancers are available and may be recommended by your healthcare provider and beneficial based on age, family history, or other factors. Early detection is especially important for cancers that currently do not have routine screening guidelines like ovarian cancer. Ruling out these types of cancers is still an important part of prevention. Keep these screening options in mind during your next appointment.
Table of Contents
USPSTF Recommended Screenings:
Other Screenings:
- Anal Cancer
- Head and Neck (Oropharyngeal) Cancer
- Ovarian Cancer
- Prostate Cancer
- Skin Cancer
- Important Note on Insurance & Billing
Disclaimer: This toolkit is for public awareness and educational purposes only. It does not replace advice from medical professionals. Please talk to your healthcare provider about what cancer screening options are right for you. Cancer screening recommended guidelines are subject to change as the science changes. Consortium staff will do their best to ensure information included is most up-to-date. Please email [email protected] with any questions or suggestions.
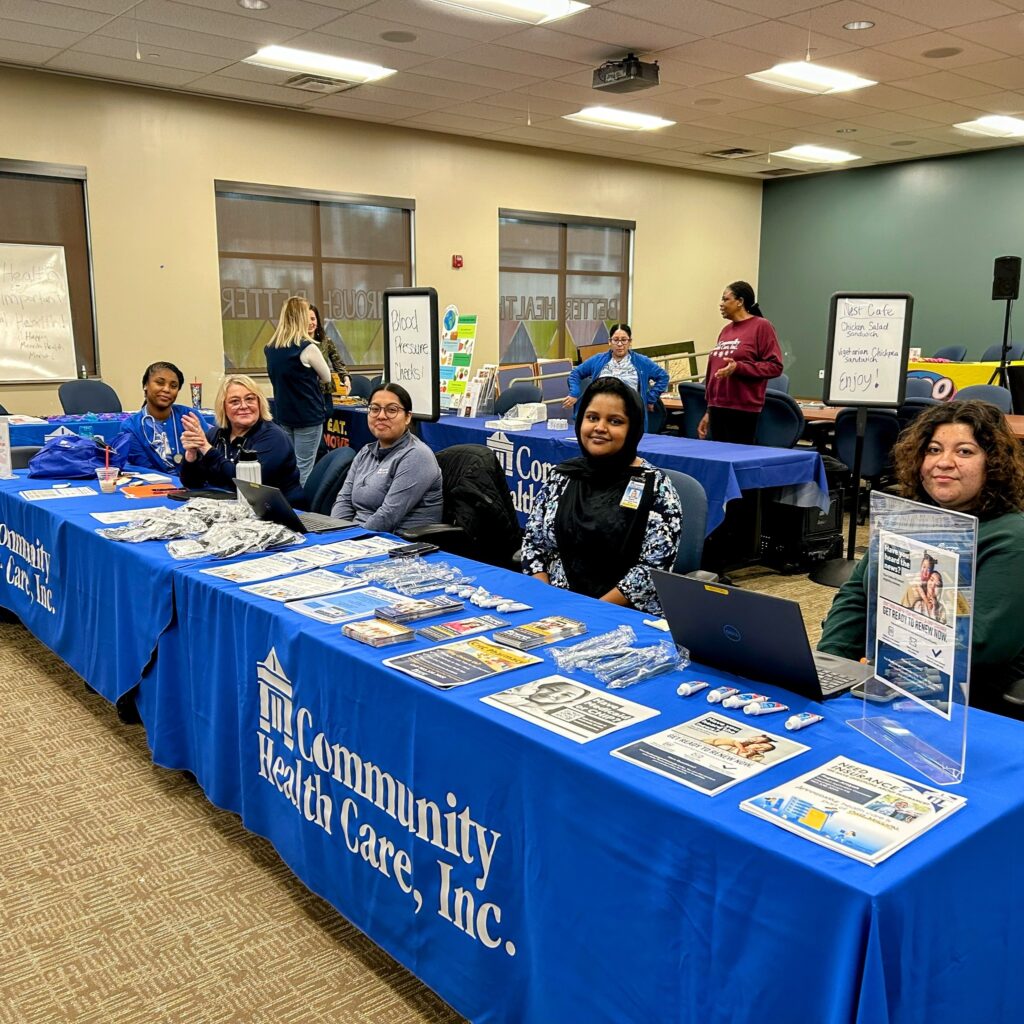
Quick Cancer Screening Guide (Rack Cards, English & Spanish)
- Full-color PDF with cropmarks and bleed, ready to be professionally printed (English | Spanish)
- Low-color PDF, ready to be printed in-house and cut, 3 rack cards per page, double sided (English | Spanish)
If you’d like to add your organization’s logo, email Liz Orton ([email protected]) for an editable Canva link.
Jump to “Avoid the Unforeseen When You Screen” cost-sharing PDF.
Breast/Chest Cancer Screening
Eligibility
The USPSTF’s recommendation is that all people with breasts* get screened every other year (every two years), from ages 40 to 74. This can include:
- cisgender women
- trans women and non-binary people assigned male at birth who have taken hormones
- trans men and non-binary people assigned female at birth
- Although top surgery significantly decreases breast cancer risk, screenings are necessary to check tissue and lymph nodes that are still there.
- intersex individuals
*Most breast cancer information is written for women, but the Iowa Cancer Consortium understands that not everyone with breasts identifies as woman or female. Cancer Research UK and Susan G. Komen have more details on breast/chest screening for LGBTQ+ patients. Surgery history, hormone usage, and sex assigned at birth can determine risk level and if/when screening is necessary (source).
Screening Methods
Common tests to detect breast/chest cancer are mammograms and clinical breast exams.
- A mammogram uses X-rays to take pictures of the breast. You stand in front of a special X-ray machine where a technologist will place your breast on a plastic plate. Another plate firmly presses down and flattens the breast while the X-ray is being taken. The steps are repeated for the other breast. It can be uncomfortable, but it only takes about 15 minutes (source). (Healthy Women Step by Step Guide)
- Tips: You will need to undress from your waist up, so some people prefer wearing two-piece outfits. Do not wear deodorant, perfume, or powder on the day of your appointment. Try not to have your mammogram the week before or during your period to avoid more discomfort.
- A clinical breast exam (CBE) is a physical exam of your breasts done by a healthcare provider to check for anything unusual like a lump. They will visually check your breasts while you are sitting up, and also carefully feel them, your underarms, and the area below your collarbone while you are lying down. You can ask your provider to perform one during your regular gynecological or annual physical check-ups.
You can also do breast self-exams to supplement, but not replace, the above screening methods.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
- Mammogram results are usually available two weeks after your appointment, and most have negative results showing no sign of cancer.
- If your mammogram does show something abnormal, you will need follow-up tests like a diagnostic mammogram, breast ultrasound, breast MRI, or biopsy–all ways of getting more detailed images of the breast–to confirm if cancer is present.
Special Considerations
If you are considered at higher-risk of developing breast/chest cancer, you may need more personalized guidelines where you are screened earlier or more often. Things that could increase your risk of developing breast cancer could include having (source):
- A BRCA1 or BRCA2 inherited gene mutation
- Li-Fraumeni syndrome, Cowden/PTEN syndrome, or Bannayan-Riley-Ruvalcaba syndrome
- A parent, sibling, or child with BRCA1/2 gene mutations or who has one of the above syndromes, who has not had genetic testing themselves
- A personal history of invasive breast cancer or ductal carcinoma in situ (DCIS)
- A personal history of lobular carcinoma in situ (LCIS) or atypical hyperplasia
- Radiation treatment to the chest at the ages of 10-30
- A greater than 20 percent lifetime risk of invasive breast cancer based on family history
To find out if you are high risk, it is best to have a breast cancer risk assessment done. Talk to your healthcare provider for more information about this tool and other risk factors.
Resources and Iowa Services
- Team Breast Friends (Benton, Cedar, Iowa, Johnson, Jones, Linn, and Washington counties)
- Especially for You Fund (Linn, Benton, Buchanan, Delaware, and Jones counties)
- Care for Yourself (Statewide) This program provides breast and cervical screening and diagnostic services, including clinical breast exam (CBE), mammograms, pap tests, human papillomavirus (HPV) tests, diagnostic testing for abnormal screening results, and referrals to treatment. Women and individuals assigned female at birth are eligible for screening. There is no cost to enroll in Care for Yourself, and participants will receive no bill for their screenings. You may be eligible, if you:
- Have no insurance or are under insured
- Experience barriers in receiving breast and cervical screening
- Have a household income at or below 250% of the federal poverty level
- Are between 40 and 64 years of age, or under age 40 with breast cancer symptoms for breast cancer screening
- Are between 21 and 64 years of age for cervical cancer screening
- Are over 64 and do not have Medicare Part B and meet income guidelines
Cervical Cancer Screening
What is the cervix?
Source: Cleveland Clinic
- The cervix is a small canal that connects the uterus and vagina in the female reproductive system. It allows fluids to leave and enter the uterus. During childbirth, the cervix widens so that a baby can be born. Learn more about the cervix here.
Eligibility
A USPSTF update is in progress, but it currently recommends:
- People with a cervix aged 21 to 29 get screened every 3 years with cervical cytology (Pap test) alone
- People with a cervix aged 30 to 65 years get screened every 3 years with cervical cytology (Pap test) alone, every 5 years with high-risk human papillomavirus (hrHPV) testing alone, or every 5 years with hrHPV testing in combination with cytology (cotesting)
Screening Method
- Cervical cancer screening tests are the HPV test and the Pap test. If these two tests are done at the same time during a pelvic exam, it is called a co-test. The American Cancer Society provides 3D examples here.
- The Pap test (commonly referred to as the Pap smear) detects abnormal cells in the cervix, usually before they become cancerous. It involves a speculum being inserted into the vagina to hold it open while the provider uses a long swab to gently scrape cells from the cervix. It is not always included in a regular pelvic exam. Everyone responds differently to the procedure, but most feel some pressure or discomfort, and the test itself only takes a few minutes.
- The HPV test, or high-risk human papillomavirus (hrHPV) test, looks for HPV infection in the cells of the cervix by high-risk types of HPV that are likely to cause cervical cancer. The HPV test can be done by itself or at the same time as the Pap test, with the same swab or a second one.
- For two days before the test(s), you should avoid intercourse, douching, and using vaginal medicines or spermicidal foam. If you had sex before the test(s), let the doctor know at your appointment. Screening tests can still be done if you are on your period at the time of your visit.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
Source: American Cancer Society
- You can generally expect to get the result(s) of your Pap test or HPV test within 1 to 3 weeks. Ask your provider’s office how they will notify you – some may call patients on the phone, while others might send a letter in the mail or update the patient’s online medical chart.
- If a Pap test or HPV test has abnormal results, your provider will order further testing to determine if there is cancer or pre-cancer. The Pap test and the HPV test are screening tests, not diagnostic tests.
Special Considerations
More frequent screenings may be necessary if you:
- Have been diagnosed with cervical cancer
- Have been diagnosed with HIV
- Have a weakened immune system
- Were exposed to diethylstilbestrol (DES) before birth
The human papillomavirus (HPV) vaccine can prevent more than 90% of cancers caused by HPV, including cervical cancer. (source)
Learn more about the HPV vaccine from the Iowa Department of Health and Human Services.
Resources and Iowa Services
- Amigas
- Cervivor
- National Cervical Cancer Coalition (Iowa Chapter)
- Care for Yourself (Statewide) This program provides breast and cervical screening and diagnostic services, including clinical breast exam (CBE), mammograms, Pap tests, human papillomavirus (HPV) tests, diagnostic testing for abnormal screening results, and referrals to treatment. Women and individuals assigned female at birth are eligible for screening. There is no cost to enroll in Care for Yourself, and participants will receive no bill for their screenings. You may be eligible, if you:
- Have no insurance or are under insured
- Experience barriers in receiving breast and cervical screening
- Have a household income at or below 250% of the federal poverty level
- Are between 40 and 64 years of age, or under age 40 with breast cancer symptoms for breast cancer screening
- Are between 21 and 64 years of age for cervical cancer screening
- Are over 64 and do not have Medicare Part B and meet income guidelines
Colorectal Cancer Screening
Eligibility
The USPSTF recommends screening for colorectal cancer in all adults ages 45-75 years old.
Screening Method
Colorectal cancer screening can be done either with a self-test that looks for signs of cancer in a person’s poop (a stool-based test), or with an exam that looks at the colon and rectum (a visual exam). Details on preparation and instructions for each option can be found here.
- Stool-based tests include a multi-targeted stool DNA test (mt-sDNA), Guaiac-based fecal occult blood test (gFOBT), or Fecal immunochemical test (FIT). Your colon sheds cells that are released in your stool, so these tests can detect any cancerous changes. You collect a sample after a bowel movement with the kit, then mail it off to your doctor or a lab. Some stool-based tests require a prescription. Ask your health care provider or pharmacist for information about which tests are available for you.
- Visual structural exams include a colonoscopy, CT colonography (virtual colonoscopy), or flexible sigmoidoscopy. A colonoscopy is most commonly used because it is widely known and covered by insurance and can allow for a full view of the colon with the option to biopsy and remove polyps at the same time.
- Many people dread preparing for a colonoscopy, but your colon needs to be cleared out for the procedure to be effective. Colorectal cancer survivors and caregivers have shared their tips for prepping here. Because you will be sedated for the procedure, you will not be able to drive or work that day and are encouraged to bring someone with you.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
- Typically, if no polyps are found during your first colonoscopy, you do not need one for another 10 years.
- If polyps are found, the next step will be to surgically remove them through a polypectomy. Sometimes this is done at the same time as your colonoscopy – ask your doctor ahead of time what they will do if polyps are found during the procedure. Depending on the type, size, and number of polyps found, a colonoscopy may be repeated in 3-10 years. (source)
- Stool-based exams need to be repeated every 1 to 3 years. A follow-up colonoscopy is scheduled if there is a positive result.
Special Considerations
While people at average risk of colorectal cancer should get their first colonoscopy at 45, high-risk groups should start earlier. This could include people who have had:
- A parent, sibling, or child with a history of colorectal cancer or certain types of polyps (starting at age 40 or 10 years before the age that family member was diagnosed)
- A personal history of colorectal cancer or certain polyps
- Inflammatory bowel diseases like ulcerative colitis or Crohn’s disease
- Family or personal history of hereditary colorectal cancer syndromes like familial adenomatous polyposis (FAP) or Lynch syndrome (also known as hereditary non-polyposis colon cancer or HNPCC)
- Radiation to the abdomen (belly) or pelvic area
Not sure if you should get screened or what screening method you should use? Know your options and take the quiz from the Colorectal Cancer Alliance. The quiz is available online or over the phone, with assistance in Spanish available.
Resources and Iowa Services
- Iowa Gets Screened (Black Hawk and Polk counties)
- Eligibility Requirements include: Iowans age 45-75 who are at or below 300% Federal Poverty Level and are uninsured or under-insured
- Educational Videos- Part 1: Your Colon, Part 2: Colon Cancer, Part 3: Screening Tests
- Free Colon Cancer Screenings and Educational Workshops (Scott, Louisa, and Muscatine counties)
- Colon Cancer Foundation of Iowa
- Colon Cancer Coalition Educational Materials
Head and Neck (Oropharyngeal) Cancer Screening
Eligibility
The USPSTF finds that the current evidence is insufficient to assess the balance of benefits and harms of screening for oral cancer in asymptomatic adults. This recommendation is intended for primary care physicians, not dental providers or otolaryngologists (ears, nose, throat specialists).
Anyone aged 18 years or older should be screened at least once a year as part of a dental exam (source).
Screening Method
- Frequent clinical examination by medical and dental providers, along with self-checks, may improve outcomes. When caught early, oropharyngeal cancers are treatable. You or a healthcare provider should do the following during a visual examination:
- Pay attention to mouth sores or lesions. If they do not get better in 2 weeks, they should be checked by a provider.
- Red and white patches, unusual lumps or swelling, and tenderness in the mouth and throat should also be monitored.
- Check the cheeks, lips, tongue (below and the sides), tonsils, roof of the mouth and the floor of the mouth.
- Palpate the outside of the head and neck as well to evaluate for any swelling and tenderness.
- Your healthcare provider may use tools like toluidine blue dye or fluorescent mouthwash with a special light to identify areas in the mouth that could become cancerous.
- Self-checks are meant to supplement, not replace, exams by a healthcare provider.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
- If the screening comes back clear of any signs of cancer, you can continue to self-check until your next appointment, which should occur at least once a year, and call if you find any changes.
- Your provider will share results with you immediately after the screening. If cancer could be present, they will refer you for further biopsy or cytology testing to get a better look at your cells.
Special Considerations
Head and neck cancers are highly preventable. Rick factors include:
- Tobacco use
- Alcohol consumption
- Unprotected exposure to radiation (e.g., sunlight)
- Poor nutrition
- Human papillomavirus infection
- Infection is preventable through the HPV vaccine. More information on the HPV vaccine and resources in Iowa here.
Resources and Iowa Services
Lung Cancer Screening
Eligibility
The USPSTF recommends yearly screening for patients 50-80 years old who:
- Have no signs or symptoms of lung cancer
- Currently smoke or have quit within the past 15 years*
- Have a 20 pack-year smoking history (one pack per day for 20 years or two packs per day for 10 years, etc.)
- Receive a written order for a low-dose CT scan from your physician
*The American Cancer Society recommends lung cancer screening for anyone who meets the eligibility guidelines above, regardless of years since quitting. Visit the American Cancer Society for more information.
There are quizzes available through the American Lung Association and Screen Your Lungs to help you determine if you qualify for a lung screening.
Screening Method
A low-dose CT scan is used to screen high-risk patients and involves no needles, medications, or pain. You lie very still on your back for about 30 seconds on a table that moves through a donut-shaped machine that takes pictures of your lungs. The entire process takes a few minutes, and you may be asked to hold your breath for certain images. A technologist will be with you and talking to you the whole time. (What to Expect– also available in Spanish and Simplified Chinese)
If you need accommodations to access screening, talk to your health care provider.
Follow-up
- If there is a nodule (a small abnormal area) seen on your scan, your physician will contact you for follow-up. It is important to know that not all nodules are cancerous, but should be watched closely by your physician.
- If you are requested to return within a year, there is the possibility of an out-of-pocket expense, especially if your deductible has not been met yet. Talk to the billing office and your health insurance provider to understand what costs you might be responsible for and if the office has financial assistance programs available.
Special Considerations
- Radon (Clinical Assessment, Radon Exposure History)
- While long-term radon exposure does not qualify a person for a lung cancer screening, radon is the second leading cause of lung cancer behind tobacco. It is important to check radon levels in homes, schools, workplaces, and other areas people gather. Learn more about radon and resources here.
- Tobacco Use Disparities
- Indigenous communities have used tobacco for religious and ceremonial purposes for centuries. However, they, along with other marginalized population groups, face greater health issues and increased lung cancer risk due to the use of commercial tobacco made and sold by tobacco companies. The tobacco industry uses marketing, flavored products, and neighborhood data to target these communities in their sales. Learn more about health disparities related to commercial tobacco here.
- Occupational Hazards
- People who work in certain environments can breathe in substances like asbestos or that cause cancer while on the job, putting them at higher risk of developing lung or other cancers. Working in industries like farming, livestock, mining, construction, first response, and the military may place you at a higher risk of work-related lung diseases like cancer. Learn more about occupational cancer risks here.
Resources and Iowa Services
Ovarian Cancer Screening
Eligibility
- The USPSTF does not recommend routine screening for ovarian cancer in patients with no symptoms or family history of ovarian cancer.
- A person can develop ovarian cancer even if the ovaries have been removed, so it is important for any person who has or has had ovaries to recognize signs of ovarian cancer.
Screening Method
- There is no standard screening test for ovarian cancer. However, if you are at high risk for developing ovarian cancer or are experiencing symptoms, your gynecologist or other healthcare provider will use a pelvic exam to feel the size and shape of your ovaries.
- In addition to the pelvic exam, there are other diagnostic procedures that are approved by USPSTF for detecting ovarian cancer, including a transvaginal ultrasound and a CA125 blood test (source). Depending on your age and reproductive status, your provider may order additional tumor marker and imaging tests.
- Keep in mind: Pap tests only screen for cervical cancer, not other gynecological cancers.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
Know the symptoms of ovarian cancer and talk to your healthcare provider if any of these symptoms persist for 2 weeks or more (source):
- Bloating
- Pelvic or abdominal pain
- Feeling full quickly or trouble eating
- Changes in bathroom habits such as frequency, urgency, or constipation
- Irregular bleeding, especially after menopause
Treatment for ovarian cancer involves a combination of surgery and chemotherapy.
Special Considerations
You may be at higher risk of developing ovarian cancer if you (source):
- Are middle-aged or older
- Have a close family member (mother, sister, aunt, grandmother) on either your mother or your father’s side of the family with ovarian cancer
- Were previously diagnosed with breast/chest, colorectal (colon), or uterine cancer
- Have the BRCA1 or BRCA2 gene mutation
- Have been diagnosed with endometriosis or polycystic ovarian syndrome (PCOS)
- Have never given birth or have had trouble getting pregnant
- Are of Eastern European or Ashkenazi Jewish heritage
- Have taken estrogen (without progesterone) for 10 or more years
Resources and Iowa Services
Prostate Cancer Screening
What is the prostate?
The prostate is a small gland in the male reproductive system located just below the bladder and in front of the rectum. It is about the size of a ping-pong ball and surrounds the tube that empties urine from the bladder (urethra). Learn more about the prostate gland here.
Eligibility
- The USPSTF recommends that for people with a prostate aged 55 to 69 years old, the decision to undergo prostate-specific antigen (PSA)-based screening should be an individual one based on its potential benefits and harms after a discussion with their health care provider.
- Trans women, non-binary individuals assigned male at birth, and intersex individuals can still get prostate cancer and should talk to their health care provider about screening options when they turn 55.
- For people with a prostate 70 years or older, the USPSTF does not recommend PSA-based screening.
- The American Cancer Society recommends starting the discussion about screening at age 50 for men at average risk and expected to live at least 10 more years.
Screening Method
Two tests commonly used in prostate cancer screening are the prostate-specific antigen (PSA) blood test and a digital rectal examination (DRE).
- A PSA blood test measures the level of the prostate-specific antigen protein in the blood. This protein is part of the semen fluid that the prostate makes. There is little risk to having the blood test, and you may have pain or bruising at the spot the needle was put in your arm. You need to avoid ejaculation for 24 hours before the PSA test because PSA levels increase when semen is released.
- A digital rectal exam (DRE) is a test in which a health care provider inserts a gloved, lubricated finger into the rectum as you are standing and bending forward at the waist or lying on your side on an exam table with knees pulled up to your chest. They are checking the size of the prostate gland and feeling the surface through your bowel wall for any abnormalities. The exam only lasts a few minutes.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
- Generally, the higher the PSA level, the more likely prostate cancer is present, but there is no specific normal or abnormal level of PSA in the blood.
- PSA levels fluctuate, but a level of 4.0 ng/ml (nanograms per milliliter) and lower is considered normal. However, there are individuals with lower levels who do have prostate cancer, as well as individuals with higher levels who do not.
- The time between future screenings depends on the result of the PSA test.
- If the result is a PSA of less than 2.5 ng/mL, you may only need to be retested every 2 years.
- Screening should be done yearly for patients whose PSA level is 2.5 ng/mL or higher.
- Higher PSA levels (between 4.0 and 10 ng/ml and greater than 10 ng/ml) can be from older age, enlarged prostates (BPH-benign prostatic hyperplasia), riding a bicycle, certain medicines and procedures, or ejaculation within one to two days of the test.
- To determine if prostate cancer is present, the doctor may recommend a second PSA blood test, a series of PSA tests and physical exams to monitor any changes, or a prostate biopsy to test a tissue sample for cancer.
Special Considerations
Because there is a risk of overdiagnosing and overtreating prostate cancer that would otherwise grow slowly and never threaten someone’s life, it is important to note risk factors that could encourage earlier screening discussion at age 45 or even 40. You may be at higher risk of developing prostate cancer if you:
- Are 65 years or older
- Are African American or Caribbean with African ancestry
- Have a first-degree relative (parent, child, or sibling) who had prostate cancer, including relatives in three generations on your mother’s or father’s side of the family
- Were diagnosed with prostate cancer when you were 55 years old or younger
- Have other members of your family that have been diagnosed with breast, ovarian, or pancreatic cancer (BRCA1 or BRCA2 gene mutation may be present in family)
- Have Lynch syndrome (also known as hereditary non-polposis colorectal cancer or HNPCC), or other inherited gene changes
- Have been exposed to large amounts of Agent Orange, cadmium, or other cancer-causing chemicals, for example, from working in the military, farming, manufacturing, or as a first responder
Take the “Am I at Risk?” Quiz from Zero Prostate Cancer.
Resources and Iowa Services
Skin Cancer Screening
Eligibility
The USPSTF is neither for nor against a visual skin examination for adolescents and adults who do not have signs or symptoms of skin cancer. The decision is left up to the medical provider and the patient.
However, a visual skin examination is recommended if you:
- Have a personal or family history of skin cancer
- Have many moles
- Have noticed changes in size, shape, or color of moles and skin growths
Screening Method
Both you and a healthcare provider can use a visual exam to screen for skin cancer.
- The American Academy of Dermatology provides information on how to perform a regular skin self-exam using a mirror in a brightly-lit room.
- During a clinical skin exam, a healthcare professional will look at your skin from head to toe. They may use a handheld device called a dermatoscope that works like a magnifying glass to inspect individual lesions (parts of the skin that look different compared to surrounding areas). (source)
You will remove your clothes and wear a medical exam gown with your underwear, unless there is a spot on your genitalia that is going to be examined. It is helpful if you come to your appointment prepared with notes on any unusual spots you have noticed, remove any makeup or nail polish, and wear your hair loose. (source)
If you need accommodations to access screening, talk to your health care provider.
Follow-up
- Your healthcare provider may choose to remove the abnormal area of skin during the screening if they think it may be skin cancer.
- They could also decide to wait and see if there are any changes after a few months or schedule a separate appointment for an excision biopsy (surgical removal).
- You and your doctor will come up with a screening schedule that could range from every 3-6 months to a year depending on results and risk factors.
Special Considerations
Anyone can get skin cancer, regardless of age or skin tone, but you may be at higher risk of developing it if you:
Resources and Iowa Services
Anal Cancer
Eligibility
The USPSTF has no guidance for anal cancer screening at this time. However, the American Society of Clinical Oncology recommends that people with a higher risk of developing anal cancer should talk with their primary care doctor about anal cancer screening. Those at higher risk who may benefit from screening include:
- People who have HIV
- People who regularly have anal sex
- People who have a history of anal warts or precancerous cell growth on the anus
- People who have a history of abnormal cell growth caused by HPV on another part of the body
- People who have had another HPV-related cancer, like cervical cancer, vulvar cancer, or vaginal cancer
- People with a suppressed immune system from an autoimmune disorder, being a transplant recipient, or long-term use of medication that weakens the immune system
Screening Method
Source: OncoLink
- Digital Anal Rectal Exam
- A healthcare provider inserts their gloved finger into the anus. This is done to feel the wall of the anus to detect any lumps, warts or ulcerations.
- Anal Cytology
-
-
- Also known as an anal Pap smear, this test collects cells from the anus to be looked at in a lab. The test is done by:
- Lying on your side with your legs bent.
- A swab (similar to a Q-Tip) is inserted a few inches into the anus. It is rubbed against the side of the bowel where the anus and rectum meet. This gathers cells from that area.
- The swab is either used to make a slide or it is put into a liquid preservative and sent to the lab.
- The pathologist looks at the cells under a microscope, looking for any abnormalities in the cells.
- Do not use an enema or insert anything in the rectum for 24 hours before the exam. Lubricants should not be used before the test because they can interfere with the results. The swab must be done before a digital rectal exam.
- Also known as an anal Pap smear, this test collects cells from the anus to be looked at in a lab. The test is done by:
-
- High Resolution Anoscopy
- In anoscopy, a small plastic tube is inserted into the anus. The inside of the anus can be better seen this way. In high resolution anoscopy, a special microscope called a colposcope is used to view the anus through the plastic tube. If an abnormal area is seen, a biopsy (tissue sample) can be taken with these tools.
If you need accommodations to access screening, talk to your health care provider.
Follow-up
Source: OncoLink
- Follow-up care depends on the result of the tests and the person’s HIV status.
- For some abnormalities, follow up will be repeat anal cytology testing a few months later.
- Some people whose results showed moderate to severe abnormalities will need treatment of the abnormal areas. Treatments can include topical medications, cryotherapy (freezing the area), laser therapy, and surgery.
- While only a very small number of people with abnormal screening results will develop anal cancer, providers have no way of knowing who will progress to cancer. Close monitoring helps to detect any cancers early when it is most treatable.
Special Considerations
Source: OncoLink
- Anal cancer is often, but not always, caused by the human papillomavirus (HPV). In particular, HPV-16, HPV-6, and HPV-11 are thought to be most related to developing anal cancer.
- The HPV vaccine protects against many types of HPV, including HPV-16, HPV-6, and HPV-11. Learn more about the HPV vaccine.
- While using condoms during anal intercourse does not completely protect against getting HPV (it is possible to get HPV with any genital-to-genital contact), condoms do reduce the genital area exposed. This can reduce the risk of HPV transmission.
- Smoking can also increase a person’s risk for developing anal cancer.
Resources and Iowa Services
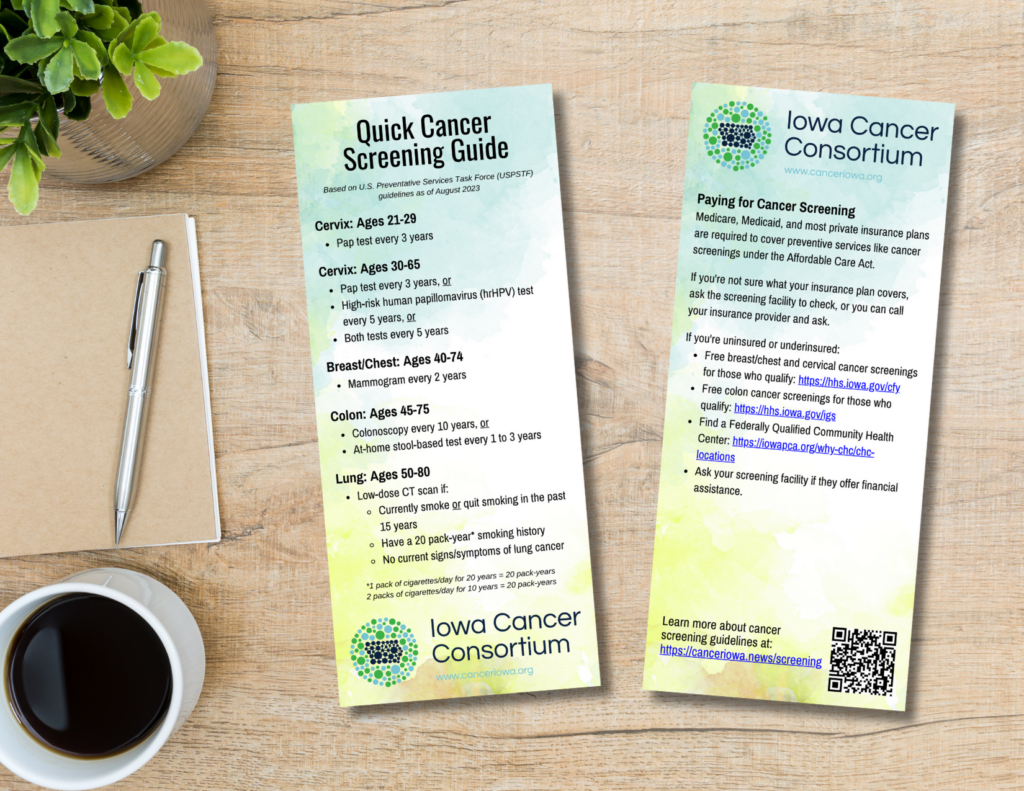
Important Note on Insurance & Billing
Under the Affordable Care Act, Medicare, Medicaid, and most private insurance plans are required to cover check-ups and preventive services like cancer screenings.
However, a preventive screening exam like a colonoscopy or clinical breast exam can turn into a diagnostic exam if you have symptoms or if something is found (e.g. a polyp or lump, respectively), which is when you may end up with medical charges. If you are unsure whether or not a screening is covered, contact your health insurance provider and ask to review preventive care guidelines to know what will be covered and what out-of-pocket costs may be.
If you are uninsured or underinsured, contact your provider or screening facility directly, since they may have funds available for your care. Iowa has programs that provide some low or no-cost cancer screenings for those who qualify. Learn more from Care for Yourself – Breast and Cervical Cancer Screenings and Iowa Gets Screened: Colorectal Cancer Program. You can find community health centers near you here.
Download “Avoid the Unforeseen When You Screen” cost-sharing flyer
If you’d like to add your logo, email [email protected] for the editable Canva link.